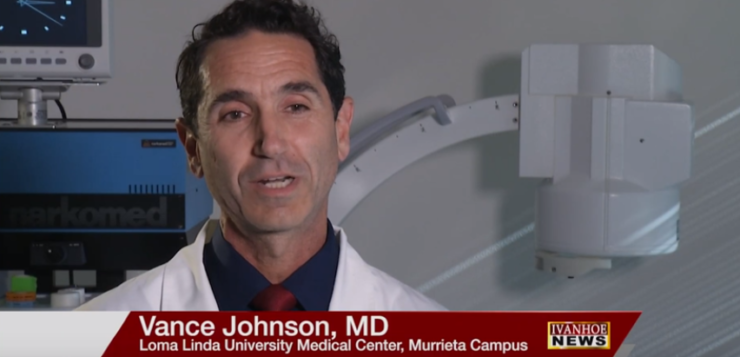
Vance Johnson, MD, Director of Spine Service at Loma Linda University Medical Center, Murrieta Campus, talks about lumbar stenosis.
Interview conducted by Ivanhoe Broadcast News in December 2018.
What is spinal stenosis?
Dr. Johnson: Lumbar stenosis is a fancy way of saying narrow. Through life our spinal canal gets smaller and smaller we start out with plenty of breathing room. There’s room for extra fluid that is nutritious for our spinal cord and our nerve roots. Through life as we get beat up and the discs collapse the spinal canal gets narrower. Usually by the time we’re sixty-five or seventy years old, the canal is quite narrow. If it gets too narrow, it chokes those structures like the cord and the nerve roots. If they get chocked, we get symptoms like aching in our back, and it might refer through the buttocks and thighs and even down the legs. And the longer we stand the more the aching and the pain continues until we go find a seat to set down on. Lumbar stenosis is a fancy way of saying chocking.
What was the traditional treatment and how did MILD improve upon that?
Dr. Johnson: Years ago, in my dad’s area, my dad happens to be a spine surgeon, retired now, but the options to him were much more limited than they are today. And that was basically to cut open the pipe, and that meant we had to cut through the skin and the muscle down to the bone and de-roof the pipe. Cut out bone and ligament to make openings in the pipe to relieve pressure. And that means scar, when you get cut you get scarred just like you see scars when you get scratched on your arm or your hand those scars form then in the areas that were cut. And that scar is now all the way down to the nerve roots. Unfortunately, sometimes those scars can encompass the nerve roots and become a problem later. And the cut is so big and cutting away muscles is traumatic, so we end up having to hurt the patient to help them and that meant long stays in the hospital and long recovers. It was common to be days or weeks in the hospital and six months or more for recovery. That was to decompress a spinal canal that was chocking the nerves. As effective as that was it was a one size fits all kind of thing. My dad’s era of spine surgeons didn’t really have the option to customize it. So when they open someone’s back they weren’t going to take out a little bit or just enough they took out the whole ligament and much of the bone to make sure that they decompressed that. And they might leave a canal that had a pressure as low as when that patient was twenty years old. But the patient didn’t need it to be done that dramatically with that extreme. Actually just a few years earlier, that patient was standing and walking without much trouble, and they didn’t need a doctor. They would really like to get back to where they were two or three years ago. Well two or three years ago, their spinal canal was only half a millimeter bigger or maybe not even that much. So wouldn’t it be great if we could customize our procedure to take out just enough tissue to make the pipe half a millimeter or a millimeter bigger? Then they’re back to standing and walking like they did two or three years ago. Well, that’s what this procedure does. It’s customized to patients, and we can see while we’re operating, actually live while we’re operating, the canal open up, and the pressure decrease. We can see the fluid passing through the tight spots in the canal. And when we see that, we know the pressure is down, and this is new for procedures for this to be able to see live while we’re operating, that the pressure has decreased. For years my dad’s generation called decompression surgery, this large surgery where we cut out only tissue but never actually measured the pressures. We used the word but there never was a pressure measured before, during or after the surgery. There was really no other evidence other than we cut out a chunk component of tissue to show that we decompressed that tight area. So, this is revolutionary in spine care to be able to see that tight canal open up while we’re operating. We can stop right there maybe have taken out only as a little as a pea amount of ligament or tissue to relieve pressure in that canal. That means we didn’t have to sew, we didn’t make a scar, we didn’t have to put hardware in there. We can just put a band-aid on the patient, and they can recover in a matter of minutes.
How are you getting in there to do that and to measure and to know what to cut away?
Dr. Johnson: It’s fluoroscopic, is the term that we use because the fluoroscope such as the one behind me, a fluoroscope is the 3-D imaging machine that allows us to see in 3-D while we’re operating. We use contrast to show where the spinal canal is that’s also a big change in spine care. Putting contrast in first means we make it safe. So unlike a procedure where we cut somebody open and we can’t really see how deep we are with the contrast in the spinal canal in the epidural space, the space that shows us where the dangerous stuff is we can stay away from it. And in a few minutes we can highlight that area and during the surgery we see that live the whole time. It actually appears on the screen as a black line. So, we stay behind that black line and know that we are safe.
And then how are you measuring pressure during the procedure?
Dr. Johnson: That’s a great question. They start off with a choke point, a bottle neck in their spinal canal. And when we put contrast in that bottleneck, it chokes away the contrast it won’t pass through. As we operate, as we take out tissue that bottleneck opens up, and the contrast passes through. And we can stop knowing that we decompressed the spinal canal. That’s the first time in spine care that we have intraoperative proof that we decompressed this spinal canal. One that is something we can replicate. I have had times when I’ve had patients come back and redo procedures on them and get that epidurogram again, and we can see that’s still open. It’s gratifying; it can really change their lives.
So is there ever a need to do it again, is it forever, one and done?
Dr. Johnson: Since I haven’t lived forever, I don’t know yet, but it certainly lasts a long time. It’s very few of my patients that I’ve gone back and repeated it. I think that the soonest I’ve gone back to repeat it is about seven years after the procedure was done.
And then even repeating it it’s not quite as invasive. What’s recovery like versus the traditional recovery? You said it could be months.
Dr. Johnson: Yeah, a typical patient of mine recovers in an hour and goes home in about an hour with a band-aid on their back. I’ve asked them to take it easy for that day, and then they can return to normal activities the next day. Normal activities for these people though is quite reduced compared to the average person. Already they’ve been stuck in a chair for a year or two or three years, so they’re not doing what most people consider normal activities. Actually, the recovery time is problematic more because of their wonderful feeling. Because of their recovery, because the feeling is so good, because of getting so much return so fast. I’m more concerned about them being too active rather than telling them what they can’t do during recovery. I’m telling them when you feel great if you feel great don’t go do eighteen holes of golf that day. Ease back in to your previous life, common sense. Because sometimes patients feel so good it’s been so long since they felt good that they really want to get back to some activity, and the overdo it.
Is there anybody that wouldn’t be a candidate for this procedure? What conditions prevent somebody from actually doing this?
Dr. Johnson: Yes, there are times when we can’t do this procedure for somebody with lumbar stenosis. If they have a tumor, if the membranes are too thick, if the bones have slipped, if they really need something else like a nerve is pinched, and they have sciatica this is not for that. If they’re facet joints, the joints in the back of the spine are collapsed, if their bones are crumbling, too soft. Those kind of things they need something different this is not for them.
If somebody has already had a big open surgery and they need something done again, can you come back and do MILD or no they’re done?
Dr. Johnson: That’s a great question. I have had that situation come up a number of times. If they’ve had the larger surgery, and they have the scar, and they’ve lost the bone and the tissue already there isn’t anything to take out there, and we don’t do this for scar. But frequently, the adjacent level is now collapsed its common particularly if we decompress and fuse somebody the neighboring joints take up the load. So, the forces get transferred to those neighboring joints, and they collapse and they might get stenotic, narrowing, chocking, and those we can treat.
With that same MILD procedure?
Dr. Johnson: With the MILD procedure. The part that hasn’t been operated on the neighboring joint.
What haven’t I asked you about the procedure that you think we should include in the story?
Dr. Johnson: The biggest, the most gratifying thing about this procedure for me and it is one of the most gratifying treatments that I offer patients, is the change in their quality of life. Lots of patients come in, and they’re very focused on their pain. If you’re hurting, if you have an ache in your back that gets worse with you’re standing and walking, and you’re standing and walking taller, and it diminishes lots of very important things you might not have considered disappear in your life. Take something as simple as a good warm hug from someone you love usually that’s done standing. If you’re sixty-five, and you have this problem in your back with chocking of the nerves you’re sitting in a chair so that means your loved ones come over, and they do this awkward stoop hug thing like that you don’t ever get that warm feeling. You’ve had to give up some independence like running your own errands and grocery shopping. You get more and more isolated you may not be going out as much with your friends; you might not be playing with that foursome or going to the church events. So you’re quality of life has dropped dramatically which interferes with all kinds of things like your mood and energy, it can lead to depression just because you can’t stand and walk for ten or fifteen minutes. It’s not really much to ask. So, people who find me or find out about this procedure that’s usually what they’re focused on. That they want to get those parts of their life back, and they want to stand and walk again. And walk just a little longer, they do want relief of pain, but it’s different from say a sciatica type of pain. The really big lose in their life are those loved ones, doing the things they love with the people they love. And all they need is maybe a millimeter more space in that spinal canal, and they get it all back. So if you have trouble standing and walking, if you’re stooping to get relief this might be right for you, and it can bring back those activates that bring meaning and joy in your life.
Let’s talk about opiate use it’s a big problem in the country and what have you noticed since the MILD procedure came in less invasive, less painful?
Dr. Johnson: Opioids are a mixed blessing and a curse. If you’re stuck with pain, and nothing helps they can give you an escape, and that can be wonderful. Unfortunately, they come with a price. If you can find another way, it can be quite attractive. Many of my patients have been using opioids to deal with the pain. Unfortunately, especially in the case of lumbar stenosis, where the spinal canal is narrow and choking the side effects of opioids particularly constipation can really add pressure to the spine and can add pressure to the spinal canal in someone who already has a chocking canal. So, it can be a real problem. But also again they still get that relief feeling with the opioid. They’re between a rock and a hard place. So, it actually can be significant improvement in their quality of life to have this procedure done, get off of the opioids, get their digestive system back, sleep better, have their metabolism return and get away from all the side effects of opioids. It’s routine for my patients to get off of opioids entirely within a few weeks after the procedure. The only reason I saw a few weeks is because we don’t want them to stop them suddenly. Frequently when they feel good they want to get off of them as badly as we want them off of them. Nobody likes the side effects of opioids, and this is a great way to get rid of them.
We were talking about stenosis.
Dr. Johnson: Lumbar stenosis is narrowing of the spinal canal, the pipe that runs up and down our spine. And when it gets narrow it can choke the structures that are in….
We were talking about what is stenosis.
Dr. Johnson: Lumbar stenosis is a narrowing of the spinal canal. If the spinal canal gets narrow you can see the nerve roots could get pinched. And so when people get chocking or this narrowing of their spinal canal they naturally want to stoop forward because when they stoop forward or sit down they get a relief. And when they straighten up to go stand and walk now everything gets chocked again. So, they end up living their life in this stooped posture, and if they stand too long and get too much pain, they have to go find a seat so that they can stoop forward and open that up. When they stand up it chokes, when they stoop forward they get relief.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
James Chisum
714-496-0541
Sign up for a free weekly e-mail on Medical Breakthroughs called First to Know by clicking here.