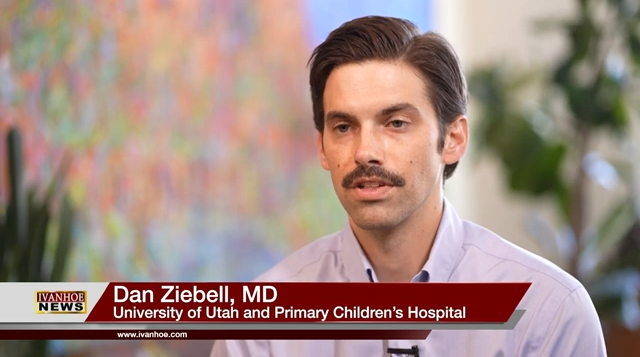
Dan Ziebell, MD, Pediatric Cardiologist at University of Utah and Primary Children’s Hospital, talks about cardiac rehab for kids.
Interview conducted by Ivanhoe Broadcast News in 2024.
When did you meet your patient Ethan Delcid?
Ziebell: So I met Ethan when he was hospitalized being cared for on a ventricular assist device. And the primary team had reached out to us because they were worried that he- was- getting- his body was getting physically deconditioned because he wasn’t being very active. And so we got involved in his care to try to improve his physical conditioning, while he was connected to a device called a ventricular assist device, which is a mechanical heart support system.
How old was he at that point?
Ziebell: So he was 3 years old when we started, and- then- and then he was 4 years old by the time we finished working with him.
When you think about this, I feel like Ethan, we’re talking about about an 84-year-old man.
Ziebell: Yeah. He sounds like he’s an old man with heart disease, but in fact, he’s a very young kid with a very complex heart disease who’s had a pretty rough go so far in a short life.
So he had to undergo cardiac fitness just to get healthy enough to get it strong enough, so he could get a new heart, right?
Ziebell: Yeah, he underwent multiple cardiac surgeries. And unfortunately, his condition worsened to the point where he needed this device called a ventricular assist device, which mechanically supports his heart because his native heart was not- doing- not doing enough work to be able to pump blood where it needs to go. And his body was suffering because of that. And then, while being connected to this device, it’s a big machine. There’s tubes that go in, tubes that take the blood out, circulate it, oxygenate it, and send it back to the heart, and send it back to the body and while you’re connected to these devices, most oftentimes kids are not being very physically active. They typically confined to their rooms or very small walks throughout the hospital. But we could see with Ethan that he was getting physically deconditioned. He was getting physically weaker. And then there were some mental health side effects of that because as any three or 4-year-old, they- they need to play, they need to be physically active. And we could see that he was having some behavioral challenges and he was struggling a bit with being confined to this machine for ultimately over a year.
Would you say that his heart really did resemble that, like an older person?
Ziebell: Absolutely. Yeah, he was he was in heart failure. His heart was not pumping blood where it needed to go and in an efficient manner, and he could not participate in activity like he needed to. As- a- year- old- like as a 3-year-old needs to.
Is a cardiac fitness center relatively new?
Ziebell: Yeah, what we do is, in cardiac rehabilitation is a concept that they’ve been implementing in adults for decades now. When adults undergo coronary artery bypass when they get stents placed when they get heart valves replaced, They undergo a physical conditioning program afterwards, and there’s really good outcomes to show that- that patients do much better once you’re physically active after a cardiac surgery. So we took a lot of those concepts and applied that to kids who’ve undergone surgery for congenital heart disease. It’s- it’s a concept that a lot of- I think there’s a lot of hospitals are trying to implement. There’s a lot of interest in doing it, but there aren’t very many centers across the country that are doing it on a large scale.
What did it involve for Ethan?
Ziebell: So for Ethan, it involved us working with him three days per week, so Monday, Wednesday, Friday. And with kids, you can’t take them and necessarily put them on a treadmill or take them to a gym and have them lift weights. But what we did is our trained team of exercise physiologists, they worked with him in a fun but targeted activities in which we were trying to keep it fun and interactive, make it seem like it’s play for him. But really what we’re doing is targeting certain muscle groups, strengthening certain areas, working on improving his aerobic conditioning.
What’s the difference from that then let’s say play therapy or physical therapy?
Ziebell: So physical therapy oftentimes is targeting specific muscle weaknesses and deficiencies, whereas we’re really trying to improve aerobic capacity. So our whole goal is that we improve musculoskeletal strength, we improve the function of the heart, the ability of the body to metabolize oxygen and circulate oxygen. Like we’re trying to improve overall aerobic capacity.
Is there a good description that you could give me of Ethan of what he was like when he was started, and then he was a year later, what he was like?
Ziebell: Well, he ended up undergoing a lot of procedures. So when we first met him he was quite physically deconditioned, and as we worked with him, he clearly got stronger. We did objective testing every 30 days where we would measure his strength and his flexibility and his stamina and every time he got better. And then towards- towards the end of the program, he ended up getting a heart transplant. And despite being connected to this mechanical circulation for over a year, he was discharged from the hospital in a matter of weeks after getting a heart transplant. Part of the reason was because he got excellent surgical care, he got excellent post-operative care. But he went into the surgery physically conditioned, and his body was stronger. And we think that that played a significant role in his ability to get out of the hospital sooner.
Is this something that you’ll do at your center for all kids going through heart failure and heart problems?
Ziebell: So every kid now who is hospitalized with heart failure gets enrolled into our program, and we’re working with every patient. So anywhere from kids Ethan size to 3-years-old up to 18-year-olds.
Do you have any stats or anything that can show how like 75% of the kids have get better?
Ziebell: I don’t have specific numbers, unfortunately. I know that all of them have shown improvements, in the vast majority of the metrics that we follow.
Do you feel like this was a pivotal game changer for Ethan?
Ziebell: Potentially it certainly played a role. I think anytime you can get a kid who’s medicalized in a setting like a hospital who doesn’t feel like a normal kid, and you give them the opportunity to feel a little bit more normal, and you give them an opportunity to play and to get stronger. I think it’s a game-changer for them.
Now, when you see Ethan, today, can you believe it’s that same little boy you saw a years ago?
Ziebell: I see him running around the hallways today, and you would never know that he has a heart transplant or that he was connected to VAD for over a year. You would never be able to tell.
Anything we’re missing?
Ziebell: It’s hard to say if he’s truly the youngest, but certainly he is the youngest at our center. And I imagine he’s probably one of the younger kids that you could possibly do a program like this on. Like, you can’t really do any structured physical fitness with a kid much younger than him. So in Ethan’s case while he’s admitted in the hospital and connected to this machine we were really focused on improving his general physical fitness. But once he got his transplant and once he left the hospital, we continued to work with him for three months. And part of the goal with that is not only to continue to build on the progress we’ve made as an inpatient. But the eventual goal is to get him to participate in activity independently, and to feel comfortable being active, but also understanding what’s normal and what’s abnormal. So when kids exercise, their heart rate goes up, their blood pressure goes up, they start breathing faster, and a kid who’s been hospitalized for over a year, when all of those things have been happening while he’s in the hospital, those are all bad things. But with exercise, when we do this in a controlled manner, we know that that’s actually a good thing. And that is actually making his heart stronger when he’s doing this on his own. And so you do have to work with kids to teach them that this sensation is not necessarily bad when you’re doing it on your own.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
Jennifer Toomer-Cook
Jennifer.toomer-cook@imail.org
Sign up for a free weekly e-mail on Medical Breakthroughs called First to Know by clicking here