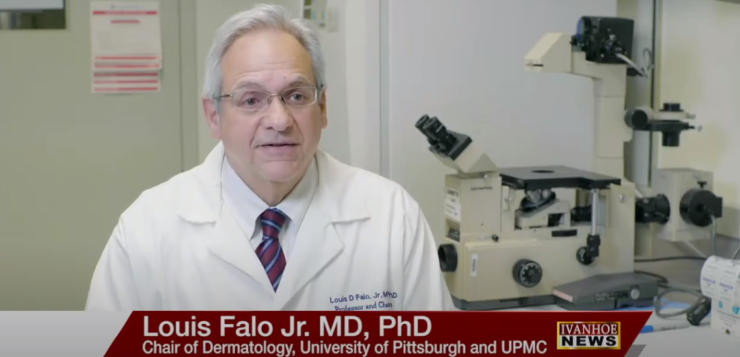
Louis Falo, MD, Chair of the Department of Dermatology at the University of Pittsburgh Medical Center and Andrea Gambotto, MD, Associate Professor of Surgery at the University of Pittsburgh School of Medicine, talk about developing a potential coronavirus vaccine.
Louis Falo: For this vaccine, we’re going to deliver a coronavirus antigen with a novel technology that’s referred to as a dissolvable microneedle array. The microneedle arrays are very unique in that they can target a specific environment in the skin. Our skin, if you think about it, is our first line of defense. It’s very well equipped to start immune response because it’s designed to protect us from invasions from viruses and bacteria that we come in contact with every day. The microneedle arrays can deliver the vaccine antigen directly into those areas of the skin that are made to make an immune response. This results in a very potent vaccine. The microneedle arrays that we use are dissolvable. In fact, the very small needles in the array are the drug. Once the needles enter the skin they dissolve and deliver the antigen cargo. It’s a high-tech device, but it’s made through a relatively simple process. It’s basically made using molding and spin casting. What is that? We take our vaccine preparation which includes the antigen and basically a sugar and load it in liquid form into molds. This solution is then spun down into the molds so that it goes inside the needle cavities and then begins to dry. In the centrifuge, this process hardens the microneedle arrays so that at the end when we pull out these molds, we have a solid microneedle array that’s resistant to outside temperatures – its very stable, does not need refrigeration and is very easy to apply. When you’re thinking about how these microneedle arrays are used in practice think about them as almost like Band-Aids. The microneedle array is simply applied to the skin topically, pressed into place for a short time, and then taken off and thrown away – the antigen is already delivered.
Does it hurt?
Louis Falo: They are painless, and they don’t cause any bleeding. The needles are very short so they’re just long enough to penetrate the outer layers of the skin so that we get good delivery, but they are not long enough to hit any pain receptors or blood vessels. When you apply these microneedle arrays, whether it’s to an animal or to a patient, the needles gradually dissolve. As they dissolve, they release the antigen. The antigen is taken up by very powerful cells that specialize in making antibody responses. These cells then travel to draining lymph nodes and start an immune response in the nodes that protects us systemically. So, the protection isn’t just skin. It’s also respiratory. There are already one or two trials in progress using microneedle arrays in the clinic, including one of our own. The application that we’re study in the clinic now is a cancer application. In that particular clinical trial, we are delivering a chemotherapeutic agent locally to a skin cancer. We would like to be able to see whether our coronavirus vaccine microneedle arrays can protect animals from being infected by the virus, but that’s not possible at the present time because we don’t have good animal models of actual coronavirus infection. Our next step will be to initiate a clinical trial. We will be doing studies that are important and necessary for FDA approval to start an actual Phase 1 safety trial to determine whether this vaccine is safe in patients. It’s hard to know when that trial will start. We hope to get the process underway soon, but in terms of enrolling patients, we must go through a regulatory process that’s necessary for approval. As we progress, there will be multiple clinical trials I’m sure with not just this vaccine but others as well. In terms of when this vaccine would be ready on a large scale for the general public, phase 1, phase 2, phase 3 clinical trials would typically stretch out to at least a year or maybe longer. In this case, the situation is different than anything we’ve ever seen so I don’t know whether there’ll be any differences in how quickly this moves forward. The major challenges now are how to scale up production of the vaccine that we’ve developed, and how to improve upon it. Also, we don’t know what the response is going to be in humans, but we know there are multiple approaches we can take to potentially make an even better vaccine. So we see this as an iterative process where we continue to develop the vaccine working through that process in animal models to develop the best vaccine for patients. I think it’s important to remember that this vaccine and other vaccines that are going to be emerging are really the result of a lot of work that’s been done by scientists in very diverse areas. We need to bring all these scientists from different areas together to be successful in this effort, and that’s what’s happening here.
Andrea Gambotto, MD, Associate Professor of Surgery at the University of Pittsburgh School of Medicine
Andrea Gambotto: The challenges are two essentially. One is to generate the vaccine that works in the first place. And the biggest challenge is to then scale up the production to the number that this vaccine is going to be eventually needed. So, this brings it back to the initial question of what the vaccine is going to look like. From the beginning you had to choose a technology which is scalable. So, you don’t want to start something that then go nowhere. We have a technology that is common technology. It’s not rocket science. It is a subunit vaccine which is relatively easy to manufacture and is scalable. We think that if immunogenicity with the combination number, the delivery system can make a possible candidate for a pandemic vaccine. So we did design the vaccine the way we did because we have a previous experience with the SARS virus in 2003 and the MERS virus in 2014. These two viruses which are closely related to COVID 19 teach us that there is a particular protein which is called spike protein, in particular a subunit of this spike protein which is called S1. It is important for inducing an immunity against the virus. So, this is the knowledge that we had when we started working on this new target that knew exactly where to fight the virus. We know the weak spot and that we had experience with the other target. And for us it was easy to switch the gear from one target to another target. We believe that this is the main target that we’re going to be looking to go after. That’s most of the group what are going to go after. Because now the literature in this site and this field brings it to this direction. So, this is the target. That is a small piece of a larger protein that the virus used to enter in the cell to a receptor. And by inducing an antibody response against this protein, you block the entry of the virus into the cell which is called in the field neutralization. So, if you can neutralize the entry of the virus in the cell, you neutralize the disease, a relatively easy task in the field of vaccinology. It’s a difficult task is do this in a restricted timeframe. This is not much different than what a flu vaccine is in terms of what you are targeting. We are targeting the protein that let the virus go inside the cell. So, it’s a well-established, knowledge established technologies that we are trying to use here. We’re just combining this technology. They’re trying to go to the next level and thinking forward in how we can learn so we can bring it into the next pandemic. Now we’re just very focused on trying to test some possible vaccine candidates. And the one that we recently developed and are trying to advance to the clinic is the best candidate that we have ever had in this same point. But for most of the vaccines, you don’t need to address scalability to begin with. But when you try to develop a vaccine quickly against a pandemic, that’s the first requirement. So, you need to call their surrogate population. So now – what’s the target population, SARS coronavirus 2? We will probably need to vaccinate all the ward because we will need to immunize the people that need that immunization, the weak people, the elderly. Probably an effective vaccine for this population would be the best but if you can afford to make a vaccine that can vaccinate even healthy people that won’t be hurt by the infection itself, their immunization will protect other people from from spreading the virus from person to person. So, the scalability to address the global city of the pandemic. If you have a virus like Ebola in an endemic area, you just need to immunize it and create the herd immunity around the area where the virus is endemic. In this case the pandemic is all over the world. So, we potentially need 4 billion of the vaccine, which we are probably not going to be able to manufacture in a short period of time. But with a few hundred million, we probably cannot trace the acute phase of this epidemic. So ideally, a vaccine needs to be manufactured in a scalable way with scalable technology. Protein is probably the most scalable biologic technology. The ability to generate the cell line that produce large amounts of data and the ability of large pharma to culture thousands and thousands of liters of media containing cells then it translates to kilograms or a pound of protein that can potentially be used to immunize a very large population. That’s scalability of manufacturing and vaccine. And then there is the scalability of packaging the vaccine into a form that is appropriate for this specific immunization. So, a limitation of a vaccine that is only a protein and has a very short life. So, you get an immunity which can be effective for six months to one year. This is the flu vaccine. Mostly you get an immunity that tends to fade down. If you have immunity induced by the coronavirus virus itself, the presumption is that this immunity will last for a much longer period. In this case, do we need more than six months? Can six months give enough time to clear the virus from all over the world? Six months would be good enough. Even three months would be good enough. And if you need that it can be administered. So, manufacturing and practicality are usually considered when you develop a vaccine for an infectious disease. But this is not the typical infectious disease for which people develop a vaccine. This is new and something that we have never faced. We never faced a pandemic in a global world where the virus can be clear and then come back after one month. So, we needed to have an instrument where we can acutely block the spread of the virus seen in the region, possibly all over the world at the same time. If not at least in the area they are interested by the endemic. The manufacturing of the of the vaccine about the spike protein is done in the cell culture. In the cell culture, the cell type is the X 293 cell which is commonly used for biological. And we transfer the genetic information of the spike protein introducing a plasmid inside the cell line. And this cell becomes. Our bioreactor in which we produce the protein that is secreted in the media? And this goes for four days. We collect the media. We do several collections every four days. And then we have liters of media containing our vaccine that needs to be dancing and purified. We use a different system for down purification – use chromatography methods to narrow down to 90-95 percent purity of the protein. And that becomes the final product that will then be packaged further. Then it comes with a needle. So now we can do the study on the SARS coronavirus 2 vaccine that we’re performing on mice. So, mice are susceptible to getting immunized. It demands an immune response against SARS coronavirus. They are not susceptible to infection with coronavirus. So, what we cannot test in this study is whether the immune response is protective. What we can learn from our study is that the vaccine that we administer to the animal – the different vaccine that we compare in this study called immunogenicity. That means we’re inducing a specific body that very likely neutralize the virus. So, after six weeks we can take the seed out of this animal, the antibody of this animal and then test the viability of this antibody to neutralize the infection. And this will eventually correlate with the potential benefit of the vaccine and on the efficacy in the human study. Usually a vaccine is tested then in a different step. Initially there is the down selection of the vaccine in the initial immunogenicity study, like the one that we perform. Then you go into an animal mold that resembles a human infection with that pathogen. The problem with SARS coronavirus 2 is that we still don’t have an animal model. We think we’re going to use the same animal model that they used for SARS that emerged in 2003. We’re pretty confident that will be the case, but we never thought that would be the case. So, in the next few months this model will become available. And we will certainly test our vaccine against this model. But we think we have enough information. Even our previous experience on the MARS coronavirus and SARS that the correlate of immunogenicity that we are observing in this early stage in the mice will eventually correlate with the efficacy of the vaccine in the model animal and eventually human. So, we really think it works to try this vaccine and advance it as quickly as possible into clinical testing because we don’t have much to lose because we perceive that this vaccine is going to be safe. It’s just a minor intervention that we’d be performing. And we are giving a pure protein for in protein. So, we don’t perceive any toxicity or side effect of this vaccine. We did immunize the mice with the vaccine, and it was manufactured using a micro needle array. And we applied the micro needle to the mouse. And we bleed the animal every week. Every week we bleed at time zero, time seven, 14, twenty-one. Every week we bleed the animal. We run in the seed of the animal within the testing to measure specific antibodies against the SARS 2 coronavirus spike. We found that the animal responded to the vaccine and mounted an immune response, so it generated antibodies that were specific for a spike. And we know that those antibodies were going to bind to the real virus. And they’re going to be able to neutralize the virus. But we can only do that at a certain time point. Usually in the first few weeks in the immune response against SARS coronavirus the antibodies are not neutralizing. As the antibody becomes better and are increased to the affinity to the spike then the antibody becomes in the 20s, neutralizing. And that’s the next step. Make sure that the antibody is neutralizing and then we are good to go.
Interview conducted by Ivanhoe Broadcast News.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
Erin Hare
University of Pittsburgh Medical Center
412-738-1097
Sign up for a free weekly e-mail on Medical Breakthroughs called First to Know by clicking here