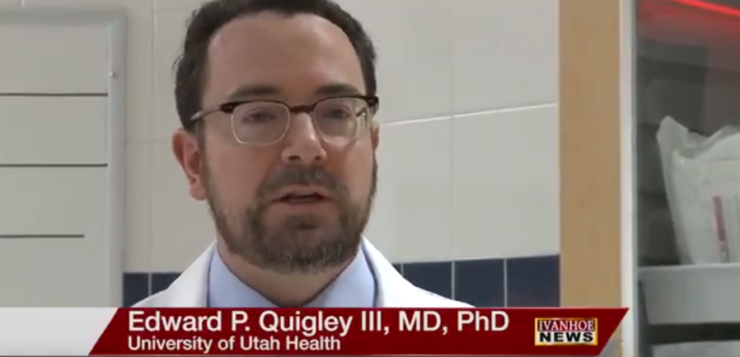
Edward Patrick Quigley, MD, PhD, Clinical Neuroradiologist at the University of Utah Radiology and Imaging Sciences talks about using virtual reality and 3D models for planning complex surgeries.
Interview conducted by Ivanhoe Broadcast News November 2017.
In this specific case you were called in to give everybody a little bit more insight, tell us how you did that, how you put together this virtual reality assistance for them?
Dr. Quigley: As a clinical Neuroradiologist, we frequently look at images in single plains, like a 2-D image or a 3-D image. In this case because of its complexity we really had an opportunity for some significant educational tools that we now have at our disposal. So we collaborated and this is definitely a multidisciplinary collaborative team, to create both virtual and physical models to help with both training education and patient education as well.
How did you do that?
Dr. Quigley: We used software that originally arose in the engineering world for taking 2-D images and creating 3-D images from them. In the automotive and aerospace industry out-of-manufacturing is the specialty of creating physical objects out of multiple small slices or out of multiple small components. Recently we’ve been applying this to medical imaging so that we can create patient-specific medical models. A nice spin off of that is when you’re creating the physical model, you can also create a virtual model that then you can load into software that takes advantage of the fact that we have two eyes. Then you can have an immersive experience with a stereoscopic head mounted display; that way you can feel right in the scan and look at that data and get a better grasp of it.
So using multiple CT scan images, multiple MRI’s, is that how you’re creating this? Tell me about that.
Dr. Quigley: We’re doing something a little bit novel; we’re taking CT’s which are based on density; things like the bones you can segment those out, we’re talking CT angiograms; studies where we give contrast to cause the vessels to light up so then we can create a model of the blood vessels that a surgeon might be dealing with. And then we’re also taking MRI data and fusing that together. So MRI can really help us detect very small areas of tumor, and in this case we were able to very painstakingly segment out all those components of tumor and then fuse those and co-register those with the bone landmarks so that there is one model that had all that information in one place.
So the information coming in is much bigger, much more in-depth than what they would have gotten had you not been involved?
Dr. Quigley: Yeah, and in collaborating with them we talked about components that surgeons or trainees would want to see. Like they would want to see a potential blood vessel or where the optic nerve was, or how displaced something was. So that sort of changed how we selected the components to build into the model.
Any surprises with what you found? I know you said it was going to be complex anyway.
Dr. Quigley: One of the things that was surprising to me as a clinical neuroradiologist was how trainees really liked this experience. The trainees who are involved had an opportunity to come in and hold the model, take a look at it from different angles, and then in the virtual model they were able to put their head into the model and look around it in a case that you know, you wouldn’t ever get to see in classic medical training, in terms of a cadaver dissection. So you have a virtual model that you can manipulate in space and see different potential surgical approaches or different relationships of the anatomy. The thing that really pulled it together is it’s patients specific; it’s this patient’s imaging turned into an educational model.
And for trainees they can go in and make mistakes and not hurt anybody. Is it to that point yet?
Dr. Quigley: Yeah, so that’s the whole area of medical simulation. One of the things we did was we printed out multiple copies of the model in a destructible model so that a trainee could practice a surgical approach on a plastic model or see how things line up. That gives us a whole area for training where then you could have multiple trainees experience through the same sort of simulator and then you can evaluate them and see how they’re doing and give them feedback. You can do that off line and in an environment where you know there’s a little bit less pressure as well.
The application is amazing for the patient obviously for training and for the surgeons themselves, it’s kind of amazing.
Dr. Quigley: Yeah. It’s a very exciting time to be a radiologist because we have the ability to bridge between what is often removed from the patient in terms of the imaging studies that are acquired. They’re complex, it takes years to train to review and learn from those images and it gives us another way to help give good answers to consultants, surgeons, and trainees.
In Jim’s specific case; what did you add to the table, what was the biggest thing you added to the table there?
Dr. Quigley: One of the things that I found really compelling was seeing him a few minutes before surgery during the patient education phase being able to hold the model and interact with it and really grasp where things were going to be going. It was surprising to me as a neuroradiologist; I don’t have a patient contact before surgery and in the OR and it was really heartwarming to see this collaborative project make a patient feel more comfortable before a large surgery.
What else haven’t I asked you that you think is important to get into the story?
Dr. Quigley: I think where the field is going is pretty important. We’re just at the beginning of this story of education and then we’re moving into simulation. As we move forward you can have patient-specific imaging that can help guide surgery, and there are implantable devices that can be 3-D printed. As we move forward anything which decreases surgical time, time in the operating room or make the trainees and residents feel more comfortable, can all help patient care. Because that’s the whole purpose of doing this is down the road to improve patient care and really make it patient-centered imaging and surgery.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
Julie Keifer
Sign up for a free weekly e-mail on Medical Breakthroughs called First to Know by clicking here