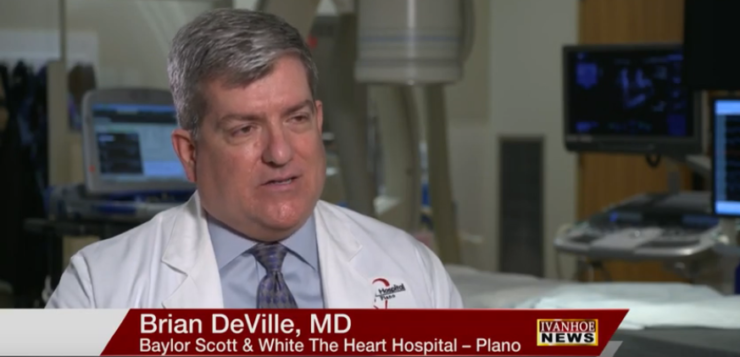
Brian DeVille, MD, Electrophysiologist at Baylor Scott & White The Heart Hospital – Plano talks about a device the size of rice, that is offering patients a less invasive option.
Interview conducted by Ivanhoe Broadcast News in May 2019.
There’s several breakthroughs involved with this story, right?
DEVILLE: There are several breakthroughs. Patients like Angela where pacemaker leads could not be placed into the left ventricle through the veins very often have had heart surgery, either an open chest procedure or a procedure where a surgeon put a scope between the ribs and affixed the leads to the outside of the heart. This has minimized the approach and is a huge first step towards making these devices smaller and completely wireless.
Making it smaller and wireless – that opens up possibilities.
DEVILLE: It really does. There are advances in leaderless pacemakers where the devices are placed completely within the heart with no incision on the chest, no wires that go from the heart to the chest wall, for example. This is another step towards that evolution.
And I guess she was in pretty bad shape. Tell us what was going on with her when you came into contact with her.
DEVILLE: When I met Angela she had undergone a defibrillator implantation at another facility by a very accomplished electro physiologist. That person was unable to place the left ventricular pacing lead in the standard manner. A few weeks later another physician attempted using another approach. That was also unsuccessful. Unfortunately in the course of this, Angela’s original devices placed in the left shoulder became infected. So when she presented to my office the pocket – the site where the defibrillator was in place, it was grossly infected. We admitted her to the hospital, started her on I.V. antibiotics and I very quickly removed the device. After that had healed up and after a course of antibiotic therapy, we brought her back to the hospital and reimplanted a defibrillator on the right side. I went in and took a look to see if we could put a lead in the standard manner and the vein that we ordinarily would put this lead in was either non-existent or closed. So we were left with a dual chamber defibrillator. At this point we were starting the wide CRT study and I felt like she would be an excellent candidate to receive this implanted left ventricular chip and the subcutaneous device that makes up the wide CRT system.
And wide CRT stands for what?
DEVILLE: The CRT component stands for cardiac re synchronization therapy. It means that we’re pacing both the right ventricle the left ventricle at the same time.
And you needed to do that?
DEVILLE: Yes. Patients like Angela who have a left bundle branch block, there is a delay between the time when the right ventricle fires and the left ventricle fires. At this point the heart is wasting energy in an inefficient manner. By pacing both sides at the same time that increases for blood flow, increases the amount of blood that the patient’s heart is able to pump. This results in alleviation of heart failure symptoms.
And it’s our understanding that this new device is like as big as a grain of rice?
DEVILLE: That’s correct. The path that goes inside the heart is roughly the size of a grain of rice. It is about that long and about the diameter of a grain of rice. It is put in through blood vessels, either an artery or a vein advanced into the left ventricle, and there is a small barb on the end of it that attaches it to the inside of the left ventricular wall. More conventional left ventricular lead is advanced through a vein on the outside surface of the heart. This one is actually Endo cardio rather than epi cardio.
How invasive was the procedure?
DEVILLE: Her procedure involved two parts. There was the insertion of the left ventricular chip device and then followed subsequently one day later by the implementation of the device under the skin. The device itself consists of the left ventricular chip. There is a generator which is the battery and the computer chips that run the device that is tunneled up under the skin, an ultrasound transducer. The device senses the pacing impulse from the defibrillator. It will also work with a pacemaker. So it senses that pacing impulse, sends an ultrasound signal that is then picked up by the internal portion. It then paces the left ventricle resulting in the two ventricles being placed simultaneously.
This would not be possible without digital technology?
DEVILLE: No, absolutely would not be. Advances in computers have miniaturized everything. When I first entered practice in nineteen ninety five defibrillators were so large they could not be implanted in the chest wall or the flank. They had to be implanted in the abdominal wall. The leads were actually very large patches that required an open chest procedure to be sewn under the outside of the heart. So things have come a very long way in the past 25 years.
They said that part of the problem with getting those leads in the right place was that her veins were too thin. Is that true?
DEVILLE: Yeah. It was unclear by the time I got there what the exact problem was. Either that vein was absent or potentially it had been damaged with one of the previous procedures. But we could not put a catheter into that vein and then subsequently advance a lead into it.
Another thing that was interesting to you and perhaps unique was the way that you were able to implant it, the way you were able to access through her groin as opposed to a vein or artery?
DEVILLE: Correct. The first iteration of the device was to put it through an artery. So we would approach from the artery in the upper leg or the groin and go backwards through the aorta, across the aortic valve and into the ventricle. That can still safely be done but it does result in a fairly large access point or large hole in the artery. So as small stature as Angela was, I was concerned about using an arterial approach and having to close the artery with that big a hole. So we went through a trans venous approach. We entered the vein, also in the upper leg or groin, and the catheter comes into the right atrium where we make a small puncture from the right side of the heart to the left side of the heart, advance a catheter and then the device is delivered from the right side of the heart across the left atrium and out into the ventricle. So this was the first trans septal placement of the device that was done in the United States.
You’re looking at a monitor? How does this work?
DEVILLE: Correct. So typically, we’re standing on the side of the patient while they’re lying on the table and we’re looking at a computer screen that has our X-ray images, our echo images and then the electrical signals from the heart. We are monitored very much like a heart cath with a few more digital recordings and enhancements.
It just always amazes me the way that you start, let’s say at the groin, and then it’s like you’re snaking up the way you want to go.
DEVILLE: True. We try to be pretty precise about the movements. Obviously we don’t want things bouncing around randomly. Once we’re in the heart we’re watching with echocardiography, either with an intra cardiac echo or with a trans esophageal echo so that not only are we looking at the X-ray image, but we’re looking at an ultrasound image that shows exactly where, for example, the tip of the needle is when we cross from the right to the left, exactly where the device is as we implant it. Then we shoot several images like with a heart cath.
What did her future look like if you were not able to pull this off?
DEVILLE: At the very least, she would have had to have a thorcotomy or a thorcostomy where a surgeon opened the chest wall and put a lead on the outside of the heart. That’s still standard therapy. This is a less invasive way of doing it. During that procedure, the incision is relatively small, but the lung does have to be collapsed in order for the surgeon to visualize the heart. With this procedure, we didn’t have to open the chest. So at the very least she would have had to have an epicardial lead placed. If cardiac re synchronization therapy had not worked on her, she would be looking at heart transplantation or left ventricular assist device placement.
And let’s say her prognosis for a long happy life?
DEVILLE: It’s really going to depend on how her heart muscle function does. We’re optimistic. She’s followed by a heart failure specialist here at Baylor Scott and White. She has done really well from that standpoint. It shows me that her activity level has increased from less than an hour a day to over three hours a day. She previously had episodes of heart failure before we implanted the left ventricular component. And those have been completely eliminated since the implantation of this device. She feels better. She is more functional. She is also protected. This device is a defibrillator, so if she does have a cardiac arrest, the device will charge up and shock her heart back into a normal rhythm. Her prognosis really looks good. All of the other options – left ventricular assist device, heart failure – heart transplantation – all of those things are still open to her if they are necessary. What we’re hoping is that we allow her to keep her original equipment and go on with a long, fruitful and happy life.
Before you could do all this, people with these problems – they didn’t do so well right?
DEVILLE: Heart failure is a leading cause of death in the United States. And people don’t realize it, but severe heart failure has a worse prognosis than most forms of cancer. So patients don’t do well unless they’re optimally treated. Fortunately medical therapies, device therapies, transplantation – all of these things have advanced tremendously in the past few years.
And then you can also check her remotely because her devices at home send you signals here at the office.
DEVILLE: Correct. We did an interrogation on her device today. We can do virtually all of that remotely from a monitor that she just keeps plugged in by her bedside. It wirelessly communicates. It does a check every night to make sure that everything is ok. Once a month we get a physiologic report on her. With that, we can tell that she hasn’t developed any heart failure, that she has not had any episodes of atrial fibrillation, ventricular tachycardia or other significant rhythms. We can tell what percentage of time she is pacing and basically make sure that there’s been no malfunction of the device or clinical episodes with her.
Right. Now this is part of a study in the United States with the device. It’s been used in Europe. What do you think of this little grain of rice device?
DEVILLE: This device is really revolutionary and it is the first device along the way to provide this sort of therapy without having to depend on leads that are mechanical devices that can fail. The device has been used in Europe and the device was available a year before it was here. There are several centers across the United States that are doing it. But it’s new technology.
Do you consider it a medical breakthrough?
DEVILLE: I think it does qualify as a breakthrough. It’s a new way of delivering therapy, and it’s another step along the way of making therapy available in a less invasive manner. We didn’t have to open her chest cavity in order to put a lead on the outside of her heart. Three very experienced electro physiologists had attempted to use a more standard approach and were unable to. With this, we saved her an open chest surgical procedure.
And everything that goes along with that.
DEVILLE: Right.
Plus you were able to get her active physically again a lot quicker.
DEVILLE: The most rewarding part of all of this is to see how she went from being extremely limited, getting short of breath walking in from her car in my parking lot into my office, and now to see that she is active and picking up and moving around three or four hours a day – it’s very gratifying when you see your patients do that well.
Are you getting a lot of satisfaction out of your work these days?
DEVILLE: Absolutely. The patients who receive CRT therapy, whether it’s the conventional approach or with this newer approach, when they’re heart failure is relieved, it’s like the governor’s taking off their engine. They’re functional. They’re happy. When you do an ablation on a patient in this rhythm problem that kept them from doing the things that they need and want to do is eliminated and they can get on with their life, it’s extremely gratifying. I tell patients our goal is to make it to where you don’t have to adjust your lifestyle around your rhythm problem. We want to correct your rhythm problem so you can get on with your life.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
Susan Hall, PR
214-820-1817
Sign up for a free weekly e-mail on Medical Breakthroughs called First to Know by clicking here