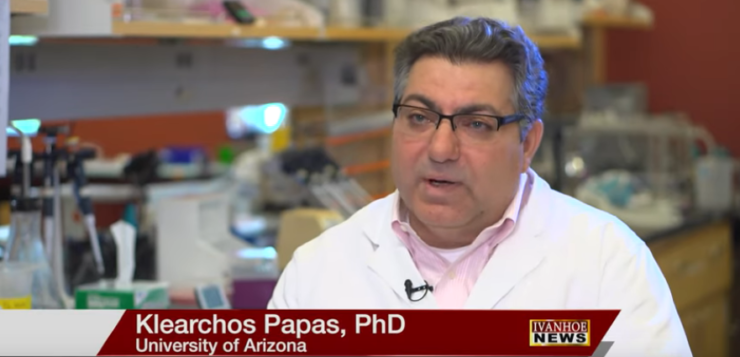
Klearchos Papas, PhD, Dir, Institute for Cellular Transplantation at the University of Arizona talks about a new teabag insulin device to help patients with Type 1 diabetes.
Interview conducted by Ivanhoe Broadcast News in May 2019.
Tell us a little bit about what the problem is you’re trying to address with the tea bag insulin.
PAPAS: We are trying to mimic what our pancreas – a normal pancreas does, and the normal pancreas has this insulin producing cells which are called islets of Langerhans that produce insulin in response to glucose. And they release this insulin minute to minute or second to second as needed. So, you don’t have a chance of going very high or very low because these cells produce the insulin. They actually sense the blood sugar and release insulin in response to that. So they have a perfect control. That cannot happen either with a glucose monitor or an insulin injection. But it can happen if you replace the cells of the pancreas that did that in the past.
That’s what your research for 30 years has been?
PAPAS: Well the research has been to be able to do this replacement of these cells without the need to suppress the immune system. I mean, part of the issue is that if you’re a Type 1 diabetic, typically your immune system will attack, for reasons we don’t understand, these insulin secreting cells and kill them, and then you become diabetic after that. If you put other cells to replace them, the immune system will also attack them. And they cannot be yours because it would also be recognized. And if there are cells that come from another donor, they will also be recognized as foreign and they will be killed. So the teabag actually separates the immune system from these cells and protects them without the need of special drugs that immunosuppress your system. So typically, you would put an immunosuppressive drug regimen to actually suppress the immune system, which has a lot of side effects and it’s a big problem. So if we can do that without the suppression and replace these cells without immunosuppression, and that’s what the tea bag would do then we can actually treat even children.
What is the tea bag? How does it work?
PAPAS: The tea bag is made out of primarily Teflon, so we use materials that have been used in humans for many years. They are safe and they can be very durable. And it has several features, but two of the key features is that it blocks cells from the immune system to get through it so they don’t reorganize them and they don’t attack the newly implanted cells. So that’s a major feature, and that’s not an easy, trivial thing. It’s many years of research on that part. So that’s the one item. The other part is that it allows glucose to go in so that these cells can sense it as they do in the pancreas and then it allows insulin to come out so that it can actually be effective in the tissues that need it. So these are two features. Then there is a third feature that it allows blood vessels to grow around it. Very small blood vessels so that they can bring the glucose to these cells and take the insulin out of the teabag and distribute it to the body. To do all that is fairly complicated, but the actual teabag is very simple. It is simple and it’s primarily made of plastic.
So, you’re testing so far in animals or strictly in lab still?
PAPAS: No, actually we have a lot of experience that we’re done in small animals and we’re now moving into large animals thanks to JDRF funding – the Juvenile Diabetes Research Foundation. Also, NIH, the National Institute of Health, has been extremely helpful with the grants. And this has been very helpful for our program to get all the way to larger animals. If everything goes well within two to three years without any additional accelerating funding just on grants, we could probably have a proof of concept clinical study with this approach within two to three years.
Where do you put the tea bag inside the body? How do you do that?
PAPAS: There are many places that we can put it. We also probably will find out as we go forward what is the ideal approach. But it could be in the arm, just under the skin. It could be in the back. It could be the abdomen. So, there are multiple locations and it probably will depend on the person or also what we find as we go forward.
You put one in and it will last the rest of your life?
PAPAS: So that also depends. But it could be one small one. It could be one larger tea bag. It could be multiple. The amount of cells you need depends on your body weight and the insulin sensitivity of the patient. So, if you have a child, maybe it’s a smaller one but as they grow they may need a few more cells to top it off. If you have a very large adult, they may need some extras. Currently the dosing at least for islet transplants, which are done under immunosuppression, is based on kilogram body weight. So it depends on the overall size of the individual, and also other factors.
Where are you getting these islets from?
PAPAS: Right now, it will be human islets from cadaveric donors, so these organs are donated and then they have to be processed. So the pancreas is about a 100 million volume – it’s the size of a water bottle – a small water bottle. But these cells in the pancreas which are spread throughout it about one to two mL. So very small volume. We purify the cells out of this large volume and we only transplant a small volume of cells. And they will be obtained from human cadaveric donors at the moment. But as we go forward there are multiple groups working on stem cell derived beta cells that can be grown in the lab. So those are the cells that we believe will treat the millions of people that need it ultimately. Right now human islets can treat maybe a few thousand people at best. And they’re also very expensive. This process will be very expensive, but as we get lab grown cells, they will be less expensive and probably more efficient and available for everybody.
What kind of success have you had with the animals?
PAPAS: We had great success with the small animals and we are getting some really good success with the large animals, but it’s very early. We were able to reverse diabetes. One of the reasons this has been around for many years is a lot of people are working on it. But it hasn’t made it to the clinic. In addition to the cells being an issue, the other issue is that this tea bag would have to be extremely large – the size of a large table top or a 40, 50 inch flat TV screen. So you can imagine putting something like that in, it’s just not practical. The major reason for that was suffocation of the cells within it from oxygen starvation. So that was the key issue. We were able to miniaturize and make this a lot more compact by providing oxygen locally. So that is one of the additions that made this work a lot better and more practical. We have been able to reverse diabetes in small animals with very high cell densities that would result in a small size teabag – smaller than a credit card, potentially, as opposed to that. And had reversal of diabetes, whereas if you don’t provide oxygen to such a densely packed tea bag, you cannot reverse diabetes. So that’s one of the things we consistently see. The other thing that is very interesting is that we see that by providing oxygen we need less cells to reverse diabetes because we make them more viable and more functional. Functionality of this size is key. Oxygen seems to be very important for these insulin secreting cells to function. So, this was something that was not as appreciated in the past, at least from many of the researchers. We have a very strong appreciation of that and we have worked to address that. So potentially we can have smaller tea bags with less cells because we provide oxygen in addition to protecting them.
So it’s working with small animals it’s working with large ones as well?
PAPAS: So far we have some very positive results. We just started. We received the JDRF funding for this large animal study, and we are working first with porcine animals. We reverse diabetes with this pig islet and then we move into human stem cell derived beta cells. And as part of that grant we received an in-kind contribution for Novo Nordisk of their cells that we will test in this animal. So these are human cells that will be used ultimately in humans, hopefully, to reverse diabetes. And we will be testing those cells as part of that JDRF study.
So human cells in the pig. That’s universal?
PAPAS: Yeah. So that’s a much more challenging model, but it’s an important model. So we use pig to pig without immunosuppression, so the tea bag can protect without immunosuppression. Human to pig is now a zeno. In the zeno we would require some immunosuppression because of the teabag but we need to do that to show that these human cells can work in the size or footprint of the teabag that it would use in a human and they would work as human cells. So human insulin and porcine insulin are very similar. The immune systems are different. But we are very fortunate that we have this model. We can do this with a teabag plus very minor immunosuppression or just regular immunosuppression. If you didn’t have the teabag and you put human cells in a pig, it’s very difficult to protect and you would need very, very exotic immunosuppression that is very cumbersome. So, we have a model that we can test human islets and stem cell derived beta cells that is simulating the human size and the form factor that is very important for these types of studies.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
Jean Spinelli, PR
520-626-2531
Sign up for a free weekly e-mail on Medical Breakthroughs called First to Know by clicking here