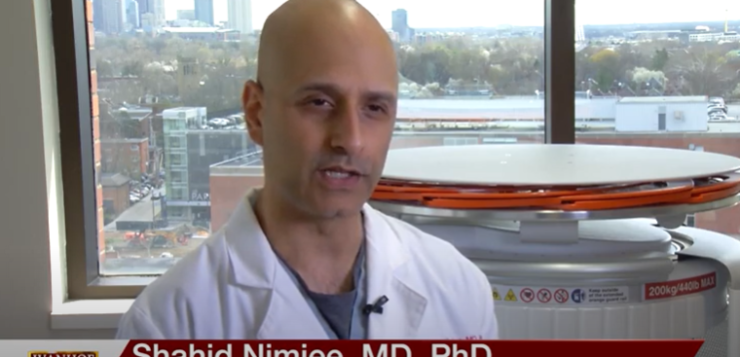
Doctor Shahid Nimjee, MD, PhD, associate professor of neurosurgery, radiology, and neuroscience at the Ohio State University Medical Center, talks about a new portable MRI machine that could possibly save the lives of stroke victims.
Interview conducted by Ivanhoe Broadcast News in 2022.
When you are having a stroke, why is time so essential?
DR NIMJEE: The reason time is so important when somebody’s having a stroke is the adage that we’ve used, which is time is brain. Neurons and nerve cells are being lost almost immediately. So, the sooner you can get evaluated and undergo the appropriate therapy for the stroke, the more brain that can be salvaged. We use an acronym that’s widely known, it’s called BE FAST. B is for balance; loss of balance is a sign of stroke. E is for eye movements. F is for facial asymmetry. A is for arm weakness, but you can include leg weakness in that as well. S is for a change in your speech, and T stands for time. If you see any alteration in your B E F A or S, you need to call 911.
What is the treatment usually? What is the front-line treatment for stroke?
DR NIMJEE: In ischemic stroke, there are only two treatments. One is pharmacologic and the other is interventional. The pharmacological treatment, which has recombinant tissue plasminogen activator, is essentially the clot-busting drug that one gets if you present within 3 to 4 and a half hours of your stroke. The other therapy, which has now been proven to be beneficial up to 24 hours after a last known stroke, is something called an endovascular thrombectomy or a mechanical thrombectomy. That’s where a doctor goes through your leg artery, or your wrist artery, gets into the brain and finds the clot that is at the base of your brain, either in your internal carotid artery, your middle cerebral artery, or anterior cerebral artery. We pull that clot out with the aid of catheters or stent retrievers in order to re-vascularize the brain again.
Is there also a time essential in that?
DR NIMJEE: We always say the sooner we can do it, the better for the patient. But that second interventional therapy has shown to be beneficial up to 24 hours after last known stroke. So, it’s opened up the therapeutic window, but only for patients who have what we call a large vessel occlusion stroke or a blockage in one of the base arteries of the brain.
How many in the U.S. have a stroke every year? How many people actually come in? And how many are here in time to get those treatments?
DR NIMJEE: So, stroke is one of those things that we don’t often think about because it doesn’t necessarily kill everybody right away. But if you think about stroke in its entirety, there’s 50 million strokes that occur every year. And as a result of those strokes, 20% die. In the United States alone, there are 800,000 ischemic strokes. When you think about our current therapeutic modalities, only about 5 to 10% of folks get the clot-busting drug and approximately only 10 to 15% of patients qualify for an endovascular thrombectomy. So, if you think about it, you have a disease that affects almost a million people every year and yet, we are only treating between 15 and 25% of those people. So, clearly, when we think about ischemic stroke and being the number one cause of combined morbidity and mortality in the world today, we have a lot of work to do.
What is HyperFine and what is it designed to do?
DR NIMJEE: HyperFine responds to the need that we need to better identify patients who could qualify for therapy. HyperFine is a portable MRI system. When we get a classical MRI or a large magnet MRI, which is approximately 1.5 tesla magnet, it allows us to image patients’ brains and any other part of the body. But with respect to the brain, it is a tool that requires scanning initially to make sure there’s no metal hardware, given the size of the magnet. It’s also a resource that is not readily available for time-critical disease at most institutions in the United States, and we’re the most developed nation when it comes to management of stroke. So, what this allows us to do is bring MRI technology to the patient rather than taking the patient to the technology or the imaging system. It allows us to take advantage of a low-field magnet of 65 milli Tesla, and the risk is dramatically reduced if not eliminated entirely. This allows us to use MRI technology to look at the patient’s own brain tissue and evaluate if they could be a candidate for thrombolytic therapy outside of the limited 4 1/2-hour window that we use today.
About how much time do you think having the HyperFine saves?
DR NIMJEE: If you think about how an MRI is used today with a patient, a patient has to undergo a questionnaire and then has to be screened with an X-ray to evaluate for implants. After that initial X-ray has been done and interpreted by a radiologist, then the patient gets transported to one of the MRI facilities within the hospital that is not located in the emergency department to undergo an MRI. If you think about our algorithm with this machine, the patient comes in with a stroke, already is scanned up to the level of their chest with the natural algorithm of stroke by virtue of CT scan. So, we already have an idea of any implants. And whether you have a question or not, it’s immaterial because then, you go straight into the MRI scanner that’s at your bedside rather than transporting the patient. And the important part of that is, as the scanner is imaging the patient’s head, those images start to come up right on an iPad for the stroke neurologist to start evaluating the tissue that is at risk and decide on whether that patient can qualify for further thrombolytic therapy. The ability to have real-time access to imaging and decide in a time-critical fashion, I think, is imperative as we move forward to treating more stroke patients.
Can you walk us through the parts of the HyperFine machine?
DR NIMJEE: Yes. So, the patient goes from the bed and slides into the machine. The head has to be in the frame, and once the patient’s in that frame, the scan can immediately start, and nobody has to leave. The patient’s family member can be beside them in the scanner. The nurses or other medical professionals can be available to the patient, so they don’t feel isolated. The scan finishes anywhere from 15 to 20 minutes, depending on the sequences that you need to make the decisions to give further therapy.
How long have you been using HyperFine?
DR NIMJEE: We started our program in November of 2021. As you can probably imagine, just like every other aspect of our society, COVID has had an impact in terms of implementing our programs that we had started almost a year earlier. So, we keep moving forward with the ambition and aspiration to make this a part of our work set in evaluating patients with stroke.
Anecdotally, what have you seen? Has it been benefiting patients?
DR NIMJEE: Yeah. So, one example I always love to give, which is a time-critical example in what I do as a surgeon, not only do we have one of these machines to evaluate patients of stroke in the E.R., but we have a second machine in our hybrid O.R., where the three endovascular neurosurgeons do most of their work. I had a patient who had a stroke and had a large vessel occlusion in the brain but also had a severe narrowing in the carotid artery in the neck, and the decision had to be made after we had opened up the vessel. Would it be safe enough to give the patient the medications we need to safely put in the stent or, in so doing, would we end up hurting the patient? So, we brought the HyperFine machine to the head of the bed, took the imaging that we needed to make a decision and, based on the images that I was able to evaluate in real time, I was able to make a decision that not only save the patient’s life but improved their functional outcome, which is ultimately the goal that we have in patients who suffer from stroke.
Is there anything else about HyperFine or about stroke that you would want our viewers to know?
DR NIMJEE: I think the important thing I’d like for people to take away is that there’s never a chance where you should think to yourself, it’s too late. If you’re having a stroke, you should call 911, get to a hospital, like ours, be evaluated with all the technology that you may not think is available, but we know is available today, so we can do the best for you.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
Eileen Scahill
Sign up for a free weekly e-mail on Medical Breakthroughs called First to Know by clicking here