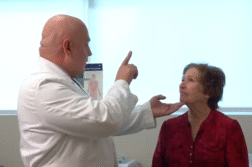
Suzanne Schindler, MD, PhD, Assistant Professor of Neurology at Washington University, talks about leading research in Alzheimer’s disease.
Like so many diseases, it is important to diagnose earlier than later. Can you explain why or what can be the difference when it comes to Alzheimer’s?
SCHINDLER: Until very recently we haven’t had any drugs approved that were thought to potentially modify the course of disease. So, we could diagnose someone early and the primary things they could do were lifestyle changes. But there wasn’t a particular drug that I could prescribe that would be expected to noticeably change the course of the disease. However, the first medication approved that is thought to potentially be disease modifying is called Aduhelm. There was a lot of controversy about that medication. There are other medications that are also in trials right now that look promising. I wouldn’t be surprised if in the next few years, we have multiple medications approved. I think that’s really going to change things in the clinic because a lot of people haven’t sought out getting a diagnosis because the idea is there’s nothing I can do about it anyway. But I think the general idea in the field is that the sooner these drugs are started the more likely they are to be helpful. The major issue is once people have symptoms of dementia that a lot of damage has already been done to the brain. So, the sooner you can get medications started the better.
And a clear diagnosis wouldn’t come unless you had a PET scan?
SCHINDLER: In the past, getting a diagnosis of Alzheimer’s disease often took a long time. First, they would go to their primary care doctor due to concerns about their memory and thinking. Then in some cases, their doctor would write them a prescription for a medication for memory. Occasionally, they would refer them to a dementia specialist for further evaluation and it could take six months to get in to see the dementia specialist. Then, we often do a thorough and painstaking evaluation that can take months to even years. The end part is to do what we call biomarker testing to confirm the diagnosis. That’s currently done with either an amyloid PET scan or cerebrospinal fluid biomarkers. However, I would say that less than 5% of patients with Alzheimer disease dementia get biomarker testing. So, their diagnosis is based on their clinical symptoms and not on any sort of testing that’s definitive. One reason is that an amyloid PET scan is $6,000 and not paid for by insurance. In terms of the CSF biomarkers, those are often covered by insurance. But a lot of people are nervous about undergoing a spinal tap which is required to do that test.
Are there other test options?
SCHINDLER: Yes. There’s a lot of advantages to having a blood test. The first being people don’t mind getting their blood drawn. It’s a lot easier than coming to a major medical center and getting an IV and being injected with a radiotracer than paying $6,000 for a PET scan or getting a spinal tap. However, at this point, I think there’s two concerns. One is that even though $1,250 for a blood test is reasonable compared to what the other tests cost, that’s still a lot of money. The other issue is that these blood tests are new. We’re still establishing exactly how accurate they are. They probably give you the same exact information as an amyloid PET scan and then CSF biomarkers maybe 85% of the time. We think they’re going to improve a lot in the next couple of years. So, my expectation is they’re going to be used a lot more.
What does the blood test show?
SCHINDLER: The blood test looks at three different factors. The first is levels of protein, or amyloid, in the blood. This is the same protein that’s in the brain in plaques. The second factor is it looks at a genetic factor called Apolipoprotein E. We know that if you have a particular form of Apolipoprotein E you’re more likely to get Alzheimer disease. Accounting for this factor seems to help us better predict whether someone has plaques in their brain or not. The third factor is age. When you combine those three factors, it improves the blood test and gets maybe 85% to 90% accurate.
Do those three factors help take the misdiagnosis out of it?
SCHINDLER: Yes, especially when people are presenting with mild memory and thinking problems. In my clinic, I would say maybe only half of the people that are presenting for the first time end up having Alzheimer disease.
What would be some of the other things?
SCHINDLER: One of the most common things is sleep apnea. Sleep apnea causes a lot of problems with attention, concentration, and short-term memory. It can be disruptive to individuals who are trying to work full-time. However, they don’t realize that memory problems are one of the most common manifestations of it. Often, people are not diagnosed with obstructive sleep apnea for a long time. So, I send a lot of patients for a sleep study. Many of them end up having a positive sleep study and get better once treated. Another common cause is medications. There’s a lot of people taking medications that impair cognition and the effects can be dramatic in some cases.
Are there a couple of medications that stick out in your mind that you always ask if they’re taking?
SCHINDLER: Sure. Gabapentin is one of the medicines I see most associated with cognitive impairment, and it’s used quite widely for treatment of pain. Other pain medications like narcotics often cause memory and thinking problems. Then also some sedative medications like Valium, Clonazepam, Ativan, and Xanax. Those are medications that if you take on a regular basis, they’re very likely to affect your memory and thinking. Now, just because they cause side effects doesn’t mean you should stop them. It just means you should discuss with your doctor the risks and benefits and do what you can to minimize the risks and maximize the benefits.
The outcome of the current study involving 158 adults over the age of 50 seemed amazing. All but 10 of the participants in the study were cognitively normal. Can you explain some to us?
SCHINDLER: It turns out that the changes of Alzheimer disease start in the brain maybe 20 years before the onset of symptoms. So, even when you look at older, cognitively normal individuals, or people who have no symptoms of dementia, we can pick out the ones that have amyloid plaques in their brains.
And if you have amyloid plaques, are you going to have Alzheimer’s?
SCHINDLER: That’s a good question and brings up one issue that we deal with a lot which is in research, we define Alzheimer disease by amyloid plaques versus most people in the lay public. They typically think of dementia and Alzheimer disease almost interchangeably. There are all sorts of things that cause dementia, and it can look very similar regardless of the cause. You can have a dementia that’s caused by medications that can look like early-onset Alzheimer disease. It’s hard to tell in some cases. We often find that people have more than one cause of their memory and thinking problems. Alzheimer’s is specifically referring to the plaques and tangles in the brain. The confusing part is that people develop these plaques and tangles in their brain for about 20 years before they develop symptoms. So, we find there’s a lot of people with Alzheimer’s disease with no dementia. But we know from following these people for years that they’re at very high risk for developing dementia if they live long enough. It’s a little bit complicated. One way you could think about it is kind of like heart disease and cholesterol. People with high cholesterol can have it for many years before they develop heart disease. They can have high cholesterol but not end up having a heart attack.
Do you think this blood test could be routine, like when you turn 50?
SCHINDLER: I don’t think we’re there yet. But yeah. Maybe five or 10 years from now that could certainly be a possibility just like getting your cholesterol checked. I think the real value of the blood test is instead of doing biomarker testing in less than 5% of patients, we could do biomarker testing in anyone that we were concerned about. And the cost, while it’s not cheap, it’s still within the realm of what we charge for other clinical tests. So, right now when I see patients for evaluation of dementia, we do blood counts, check their thyroid, and check their B12 level. We do not check their amyloid level. I think with this blood test, we could start doing that because it would be helpful information. I personally think it’s very odd that in patients who are presenting for memory and thinking problems that we don’t do a test for Alzheimer’s disease when we have one available.
What do you want people to know about, or what excites you about the research right now?
SCHINDLER: I think this is what excites me about it. People have had Alzheimer’s disease for probably all human history. There’s just this expectation that when you get older, you’re going to become senile and develop dementia. This research is giving us hope that one day we’re going to be able to prevent Alzheimer disease. I’m hoping that I’ll live to be 100 and be sharp as a tack, and I hope that for everyone else.
Interview conducted by Ivanhoe Broadcast News.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
JUDY MARTIN FINCH
314-286-0105
Sign up for a free weekly e-mail on Medical Breakthroughs called First to Know by clicking here