Dr. Shankar Rajeswaran, MD, Division Chief of Pediatric Interventional Radiology at Lurie Children’s Hospital, talks about unicameral bone cysts in children and a new treatment for them.
Interview conducted by Ivanhoe Broadcast News in April 2022.
UBC. Tell me what a UBC is.
DR RAJESWARAN: So a UBC is a unicameral bone cyst. Essentially what it is, it’s a benign bone tumor. So it replaces normal bone and it’s a fluid-filled cyst that expands the bone, makes the bone thinner. And so then the walls essentially become as thin as an eggshell. And then a child is essentially prone to fractures.
Does it only happen in children?
DR RAJESWARAN: Primarily in children. Young adults can also have it.
Is there anything – any reason? Is there any cause?
DR RAJESWARAN: We don’t truly understand what causes UBCs. And the incidence of it is about 1 in 10,000 kids.
And once you get it, do you get them your whole life?
DR RAJESWARAN: So some kids will be asymptomatic from UBCs and they’re just discovered incidentally. So say a child falls and then they take an x-ray and they may see a cyst at another location. Sometimes as a cyst is expanding it can cause pain and occasionally it can fracture.
And so how do you usually treat these cysts?
DR RAJESWARAN: So in cysts that are symptomatic, cysts that have fractured or cysts that cause pain, a surgeon may go in there with a surgical incision, scrape the cyst wall to destroy the cyst, and then may put an artificial bone in there to help the cyst heal in or may use metal plates and screws to stabilize the bone.
Now, before we go on any further, let’s talk about it. Do all of these bone cysts usually end up in multiple fractures?
DR RAJESWARAN: So at times when a child initially fractures, someone may choose to just watch the cyst, hoping that it heals in. Some children may not fracture again, and some may.
So you’re talking about treatment for it. Is it pretty easily diagnosable?
DR RAJESWARAN: It’s pretty straightforward. On an x-ray, essentially, you normally are used to seeing normal bone. But in the setting of UBC, you’ll see a cyst filling it and you’ll see the walls thinned out, like I said, kind of looks like an eggshell almost.
And so bone grafting is a part of also how you help these children?
DR RAJESWARAN: Correct. So when a surgeon goes in, as they scrape the walls to destroy the cyst they put in this artificial bone to help expedite bone healing.
But is it pretty invasive, then? It seems like it’s an open surgery.
DR RAJESWARAN: It’s an open surgery and it’s invasive. And there are still recurrences associated with open surgery.
And why is that?
DR RAJESWARAN: We don’t really know- it falls within the family of bone tumors, but it is benign and you can have recurrences. And unless you kill the cyst in its entirety, it’s going to come back.
And now you are using a new way to take care of this.
DR RAJESWARAN: Yeah. So this was back in 2018 or so we thought about a way to do a minimally invasive approach to treat unicameral bone cysts. And so rather than doing an open incision, we asked ourselves, can we treat this with needles? And so through two small pokes, we get two needles into the cyst and we inject a medicine to destroy the cyst. And via those two small needles, we then inject the bone graft. And thus far, our results have been really promising over the last four years.
What’s the medicine?
DR RAJESWARAN: The medicine we use is something called Doxycycline. And it’s an antibiotic, but when it’s inside tissue it can destroy the underlying cells.
Which seems better than before. I was reading, I think that a lot of the treatments before might involve steroids. And I think people, you know, always say steroids, oh, you don’t really want to use them. Is that correct?
DR RAJESWARAN: So yeah. Folks were injecting steroids, but the recurrence rate with steroids were pretty high. And secondly, the difference with our technique is we destroy the cyst with the Doxycycline, but we’re also injecting the bone graft, which helps expedite healing as well to strengthen the bone. And so at a few months, the bone looks pretty good and kids are able to return to activity much quicker.
Is it like one and done? One antibiotic injection and done or?
DR RAJESWARAN: So once we get the needles in, we inject the medicine, the Doxycycline, and then we inject the bone graft. And we do have recurrences, just like open surgery does, but thus far our results are comparable to open surgery and maybe even better.
And a lot better recovery, right? There’s no recovery, is there?
DR RAJESWARAN: Well, afterwards, because the incisions are so small, it’s just a Band-Aid. And so kids feel pretty good by the next day.
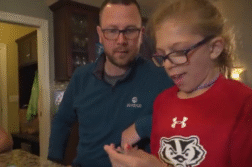
Can you tell me a little bit about Brooklyn?
DR RAJESWARAN: Yeah, so Brooklyn’s story is really interesting because she was the first kid that we actually used this technique on. It was back in 2018. Prior to that, she had fractured and she had seen a surgeon who had done an open incision, scraped the cyst wall lining and then grafted it. But she had a recurrence. And at that juncture, she was told that there wasn’t much more that could be offered to her and that maybe when she was an adult that the cyst would go away. And so she was told – I think at that time she was about 9 or 10 – no contact sports or strenuous activities with that arm until she’s an adult.
That’s horrible.
DR RAJESWARAN: Right. And so that’s when the family came to Lurie seeking a second opinion. And in conjunction with Dr. Peabody, who they initially saw, who then referred Brooklyn to me, we proposed this novel technique, which was, let’s inject the medicine to destroy the cyst and then inject this bone graft via needles. Yeah. And Brooklyn is now four years out. She actually got x-rays today, and her arm looks pretty normal.
Does it – like, is she allowed to do anything now?
DR RAJESWARAN: Yeah. She’s back to normal activity.
Yeah?
DR RAJESWARAN: And that was – she was back to normal activity within a few months.
So you’re changing these life for these kids. You’re giving them a childhood, really – like a normal childhood.
DR RAJESWARAN: Yeah. Kids are ecstatic, especially when you’re told there’s not many options. And the fact that it’s so minimally invasive, after the fact, when you see them, when we see them in clinic afterwards, you can’t even see the scars that we’ve gone in because we’ve used needles that previously required an open incision.
So are you doing any open surgeries now for this?
DR RAJESWARAN: I am a pediatric interventional radiologist, so I do everything using pinhole incisions. So – and at Lurie, the majority of kids are getting this procedure done.
But this is one of the few hospitals that are doing this right now, right?
DR RAJESWARAN: Yeah. We came up with this technique and it is slowly gaining traction around the nation. But most places around the country, it’s still being done by open surgery. Well, we hope that changes in the next few years.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
Julianne Bardele
(312) 227-4265
Sign up for a free weekly e-mail on Medical Breakthroughs called First to Know by clicking here