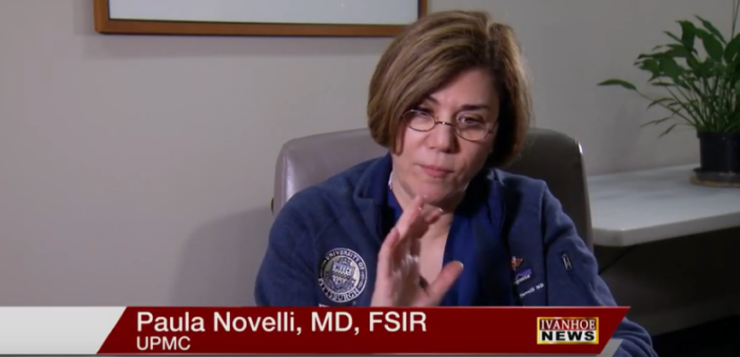
Paula Novelli, MD, FSIR, Associate Professor of Radiology, Division of Interventional Radiology at UPMC talks about the RenovoCath and how it is helping doctors and patients.
Interview conducted by Ivanhoe Broadcast News in May 2019.
You said you’ve been an interventional radiologist for 20 years?
NOVELLI: Not quite, since 2004. I trained here at the University of Pittsburgh as a resident and as a fellow. Here, we have extensive training in treating pancreatic and liver disease.
Do you have people coming from around the country? Are there other centers? How many other centers?
NOVELLI: I think there are 30 sites participating in the trial. Medical and surgical oncologists treating pancreaticobiliary cancer treat these patients with unresectable pancreatic cancer with referrals from everywhere. As interventional radiologists our involvement in treating these patients has traditionally been placing venous ports for systemic chemotherapy, relieving biliaryobstruction or jaundice s, treating complications of therapy, and we’re doing stuff at the end of life for these patients such as palliative feeding tubes and drainage catheters. This is our opportunity really to have a front-line therapeutic role. And that’s great for us and for these patients. We’ve provided local regional therapy in the liver for decades. So, this is our first opportunity to actually provide locoregional therapy within the pancreas . This is a treatment option that has really shown to have significant clinical benefit, and we’re encouraged, the patients are encouraged.
What is it that you do as an interventional radiologist?
NOVELLI: An interventional radiologist is a essentially a minimally invasive surgeon. We make tiny incisions in the body and use X-rays or radiology to guide us . We treat many conditions. We treat essentially anything from blockages and bleeding in blood vessels or bile ducts and most organs We deliver chemotherapy through blood vessels. We treat traumatic bleeding. So essentially, we treat any organ or blood vessel in the body other than the heart or brain.
Can you talk a little bit about your role when you’re dealing with cancer patients up until now?
NOVELLI: I have been treating primary and metastatic disease within the liver. I treat hepatocellular cancer or primary liver cancer, metastatic breast, metastatic , colon , bile duct and other cancers that spread to the liver. We can treat essentially any cancer in the liver by delivering chemotherapy directly to the tumor via the artery. This is new treatment is different for us in the sense that we’re actually delivering the therapy to the pancreas locally instead of locally within the liver like we have been doing for other types of cancer.
What does that do for you? Do you feel like you and your team are now on the lines with this particular cancer?
NOVELLI: Absolutely. Our surgical oncology colleagues and medical oncology colleagues have been delivering systemic chemotherapy or resecting early stage pancreas tumor patients. But with this sort of subset of patients that’s locally advanced, the options are limited. And for us to be able to treat in ways that we’re familiar with in other organs is exceptional. And I think that it’s encouraging for us to be able to expand our clinical presence and therapeutic benefit to this subset of patients.
Why is pancreatic cancer so tough to treat?
NOVELLI: Most patients will present at an advanced stage. We know that resection is really the only chance for a cure for these patients. For the patients that don’t meet resection criteria it’s essentially a death sentence. When we hear pancreatic cancer your immediate reaction is dismal. That is because we have not been able to offer any treatment that had a significant therapeutic or clinical benefit as interventional radiologists. The early studies with the treatment that we are able to offer through this clinical trial has shown to increase survival from 11-14 months to 26 months and longer. 26 months is absolutely huge. If you look at a clinical trial in medical oncology, a positive clinical trial can be an additional one-week survival benefit or time to progression of the cancer a week to a few weeks. We have a patient who’s living three years out. Our longest survivor at this point but still counting. To give somebody who’s diagnosed in November a year’s survival beyond the following October that they are not expected to live past is great. Now for these patients when 11 months comes, they are going to wake up the next day. For most patients innthe several months leading up to end of life , they not living well. They are dwindling and often in the process of dying. With this therapy, this is a 11 plus month process of living, living better and longer
You say 14 and then 26 months. What does that mean for somebody like Darlene?
NOVELLI: It means that she’s going to have the opportunity to fulfill more dreams and enjoy more interactions with her family, and just life in general. When you see patients that are progressing along with their chemotherapy regimens, those patients are obviously sick. No matter how well tolerated it is systemically there are systemic side effects. With this therapy, I think she’s absolutely indifferent to it. She’s on an antibiotic for pre and post procedure. I call her a few days after the therapy because she is in every other week just to see how she is in the interim. She’s doing well. She has no symptoms from treatment.
Talk to me about this procedure and what is making the difference why Darlene look so good.
NOVELLI: The name of the trial is the Renovo Tiger- PAC trial that allows us to treat patients who are already receiving systemic chemotherapy and radiation. Our subset of patients continue additional treatment with this local regional therapy. We’re adding this to the systemic chemo radiation regimen. They’ll complete four months of chemo and radiation therapy; then they’ll move on to our treatment for four months for a total of eight treatments every other week. The subset of patients in the other arm of the study will continue with systemic therapy. They all have received the systemic chemotherapy; they have been radiated locally. Our new treatment allows us to really douse the tumor if that’s a good word or sort of drench it with this chemotherapy directly to the site of cancer. We do deliver chemotherapy in the liver arteries for primary and metastatic diseases in the liver. We’ve never been able to deliver it to the pancreas. The blood supply to the pancreas is quite different than the blood supply to the liver. We needed a way to deliver that drug to the tumor in a way that was different than by using the standard catheters that we have.
What does this allow you to do? What will we see while we’re in the operating room?
NOVELLI: You’ll see that this type of catheter is able to isolate segments of the blood vessel and force chemotherapy through the vessel wall into the tumor. So, you can treat a tumor that predominantly not too vascular or has a blood supply that we can’t detect on an angiogram so well. We actually sort of bathe any tumor in proximity to our catheter. We’re actually forcing the chemotherapy into the tumor as opposed to spraying it on the outside like we would do in the liver.
Could walk my viewers through what you technically do.
NOVELLI: We’ll place a catheter through the groin in the femoral artery, very similar to a cardiac catheterization but we stop below the diaphragm and put our catheter into the main artery that feeds the pancreas. This come off a blood vessel called the celiac artery. We’re able to, with our catheter in place, take pictures of the blood supply to all to where we see tumor on the CT scan or MRI. We know where we can expect the blood vessels to be and we’ll park our catheter in a region where we think most of the tumor is in close proximity. And then we’ll isolate that little segment of blood vessel. There are little balloons on each side of the catheter. This way we blow up the balloon so no blood flow can get enter the segment past the first balloon and no blood can flow out past the second balloon. Once this little segment is isolated, we pressurize the that vessel with this chemotherapy and it will reach the tumor through the vessel wall. It doesn’t do any harm to the vessel wall. It’s completely angiographically intact when we’re done. It’s quite effective. When we looked at her cancer tumor numbers and for me as a radiologist, what this tumor looked like on her follow up imaging, I was shocked and quite happy.
How do you know that this is making a difference? Can you describe what you see?
NOVELLI: We see significant reduction in the bulk of the tumor, and, not just the tumor morphology, but the effect the tumor has on adjacent structures. So, structures that may have been compressed or impinged upon are freed. They’re not encroached. I’m an interventional radiologist so I rely on my diagnostic colleagues to actually interpret images a little bit better than I can but even I could see the improvement. I was asked to show Darlene her images and a lot of times as a radiologist you’re pointing something out, and maybe it’s a little bit subtle for a layperson to see or even for me to see, but I took pictures of before and after and it was something that my 12-year-old daughter would show you and say this is bigger and this is smaller. So, it’s actually something that’s not subtle, it’s a marked improvement. I think we’re only going to see more improvement with subsequent scans.
What is Darlene’s prognosis then? Will there come a time when this won’t be effective?
NOVELLI: Well, I think that those are our early numbers. And like I mentioned; we have somebody who’s three-years-plus you know three-years-plus from when we initiated her therapy. We’re encouraged by that. We don’t know what the future holds, but I think that she’s doing very well. I think that when she’s out and about at the grocery store or at a restaurant, you won’t know that she’s sick. I think that this is what’s very encouraging, not just the therapeutic benefit but we’re able to treat this tumor locally with significant clinical effect and keep the patient healthy and living throughout the therapy, which I find encouraging. This is the reason why we’re so happy and grateful that we’re able to participate in this trial.
Is there anything I didn’t ask that you want to make sure that people know?
NOVELLI: It’s nice to sort of create some awareness that we’re able to offer this. And of course we want every medical center to offer this. We’d like to show that there is significant clinical therapeutic benefit.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
Cyndy Patton, PR UPMC
412-415-6085
Sign up for a free weekly e-mail on Medical Breakthroughs called First to Know by clicking here