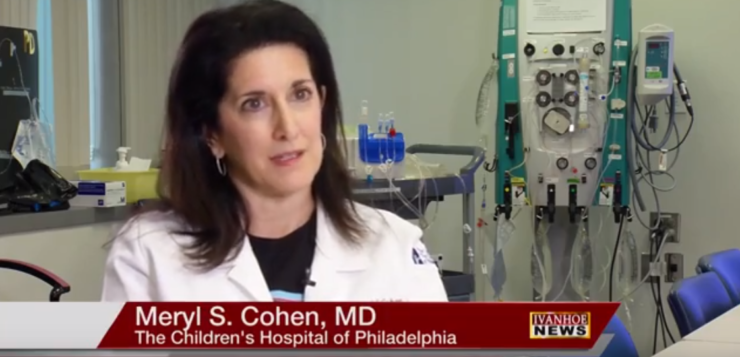
Meryl S. Cohen, MD, Professor of Pediatrics at The University of Pennsylvania, Perelman School of Medicine, Associate Chief, Division of Cardiology at The Children’s Hospital of Philadelphia talks about stokes in kids.
Interview conducted by Ivanhoe Broadcast News in July 2018.
Profess of Pediatrics in the Division of Cardiology at the Children’s Hospital, Philadelphia.
We were talking earlier, it’s not that unusual for a child of this age to actually have a stroke like this?
Dr. Cohen: Well it is unusual, we tend to see it here at the Children’s Hospital of Philadelphia because we tend to see unusual things but it’s certainly not as unique as you might think. We always think about strokes in much older individuals but occasionally it happens in young children as well.
Medically you were talking about how tenuous the whole situation was because you had to make sure that the tumor wasn’t there and you had to do all of these things at once to make sure that it turned out okay.
Dr. Cohen: Correct, John had what looked like a small tumor on his mitral valve which is the valve between the upper collecting chamber on the left side of the heart and the pumping chamber on the left side of the heart. And even though it didn’t look particularly large our concern was that it was very mobile and that it could get released and go to bad places. And one of the bad places it could go is to your brain. And if it goes to your brain it will block a blood vessel and cause a stroke. And John had already had a stroke and that’s what led to him have a cardiology evaluation to see if there was something in the heart that was causing him to have had that stroke.
So by the time you got in there and did the exploratory surgery was the tumor gone completely?
Dr. Cohen: Almost all of it, there was a very small piece left on the mitral valve that Dr. Massio our cardiothoracic surgeon here was able to remove. Our concern was that if any remnant was left on the mitral valve that he was still at risk for having another subsequent stroke and we didn’t want to leave him with that risk.
A tumor you think of as being stationary, why is this one mobile within the body?
Dr. Cohen: This one is called a papiilary fibroelastoma and that sort of terminology means that it’s a very sort of fibrous string like tumor. It doesn’t look like a typical sort of solid mass. It is very mobile and it tends to attach to valves and when it attaches to a valve it can go in and out of the chambers of the heart. And the blood flow can pull it and possibly break it off and that’s probably what caused his initial stroke.
So running through medically what happened, he faints, they bring him in and obviously a very happy ending. But medically can you walk us through exactly what happened that led up to that?
Dr. Cohen: Sure. After he had that event he had a CAT scan and was noted to have had a stroke. Once you know that somebody has a stroke you see if it’s what we call an embolic stroke or a hemorrhagic stroke. Embolic means that something blocked the vessel, hemorrhagic means that you bled somewhere in your brain. So his was an embolic stroke and then you have to start looking to see if something could have caused that. And one of the areas we always look to see for a cause is in the heart. You could either have had a blood clot in your leg that gets to a small hole in the upper chambers of your heart and gets to your brain. Or you can have a tumor in your heart that leads to this. John had gone to see a colleague of mine In New Jersey, she had done this echocardiogram of his heart and saw this structure on the mitral valve and didn’t know what it was. So she sent the echocardiogram to me and when I received it on a Monday afternoon I realized it was likely this papillary fibroelastoma and we had experience with other patients who had significant consequences of having this type of tumor in their heart. I called the father and asked him fairly urgently to come down to talk to undergo evaluation. We brought our neurologist in, Dr. Daniel Licht, who also was involved in this process. We did further evaluations of him and decided that the best course of action was to take the tumor out. When we brought him to the operating room we wanted to do something called a transesophageal echocardiogram to get a better look at the tumor. The patient is anesthetized so John was asleep. We put a probe down his throat and did an ultrasound of the heart at that time. And what we noticed was that the tumor appeared to be gone. We no longer saw it which meant that it had embolized or moved away from the heart to somewhere else. And that somewhere else could have been his brain. So we were very concerned about that and Dr. Mascio the surgeon and Dr. Licht and I were sitting in the operating room trying to figure out what to do. And we decided the initial thing we had to do is make sure that it had not gone to his brain. So we took him anesthetized with our cardiac anesthesia team down to the CT scanner and did a brain scan again to assure ourselves that the tumor had not gone to his brain. And fortunately it had not. We actually don’t know where it went but it appears to have not gone anywhere harmful because it did not have any evidence of disease anywhere else in his body. And we brought him back to the operating room. Then we had to decide whether we needed to do an exploratory operation which is still an open heart procedure and not without risk to remove anything that might still be there. The other option was to leave it alone and see if it comes back. So the three of us went down to meet with John’s parents who had to make a very difficult decision with us. And we all thought the best course of action was to do this surgery to make sure that there was nothing left on his mitral valve.
And you think it just disappeared or broke up?
Dr. Cohen: It probably broke up somewhere in his body in a very benign way so that it didn’t cause him any harm. When Dr. Mascio went in to do the operation you could see where the tumor had been anchored there was still tissue left there on the mitral valve. And so Dr. Mascio removed that tissue that had been there to assure that there was nothing left. Fortunately when we did the transesophageal echocardiogram after the procedure you could see that the mitral valve was working normally, his heart was working normally there was no evidence of residual disease. And we were able to take him safely back to the cardiac intensive care unit for his recovery.
Do you have any idea how that tumor started?
Dr. Cohen: It’s completely unknown. We don’t know why these happen. They’re exquisitely rare but we have had a handful of patients here who have had these types of tumors and we almost always feel the need to remove them because of our concern that they will embolize which means that they will break away and go to potentially bad places.
So what happened with him, he fainted?
Dr. Cohen: Right.
How lucky did he get that it happened and you guys were able to find it?
Dr. Cohen: Yes, I would say there is definitely always luck involved in these things. Fortunately he had a warning signal rather than a really tragic event. If that entire tumor had gone to his brain it’s likely that it would have blocked off a very major vessel because it could have potentially blocked of an entire vessel and he could have had a much larger stroke which would have been very consequential for him at such a young age, for anyone actually. Fortunately his stroke was very small and essentially it had no consequences from it so he’s been okay.
Just a question about was it a piece of the tumor that caused the stroke? A little bit of it broke off and clogged?
Dr. Cohen: That’s what we presume. We honestly don’t know for sure. But we know that if you see something in the heart and the patient has had a stoke you can surmise that a little piece of it has broken off and gone to the brain and caused a little obstruction of a very tiny blood vessel. When it’s a very small piece it goes to a very small vessel it gets stuck in there and that’s when you lose the oxygen beyond that little vessel.
Is he good now, he’s fifteen, so he’s going to have a good life?
Dr. Cohen: Yes, I would expect so. We’ve advised him not to play football for other reasons.
This is a ton of pressure on you guys. You’re in the OR and he’s under, you’ve got to run down to the CAT scan and it’s a kid. As a doctor how do you do that?
Dr. Cohen: That’s our job I guess, I don’t know. What we always have to do is weigh the risks and benefits of everything we do and we’re often dealing with very significant issues with patients. In cardiology in particular there’s a lot of life and death things that occur. We wanted to do just what we thought would be the best in the long term for him. We knew there was risk of doing this operation because when you do any cardiac operation on someone there’s a risk that something can happen. You can stroke just from the operation. Just from being on the heart/lung machine. And so we knew that there were those risks. But I think honestly with the help of the neurologist Dr. Licht and Dr. Mascio knowing confidently that he could handle this that we felt that the best course of action was to put him under this small risk of the operation with the idea that the benefit would be that this thing would be gone, he wouldn’t have to think about it anymore. It wouldn’t be hanging over this family’s head, it wouldn’t have a chance of growing back and he would be able to go on and do all of his normal activities that he wanted to do, including football if he wanted to do it for the rest of his life.
Did I leave anything out that you wanted to talk about?
Dr. Cohen: I don’t think so. They were really just a very lovely family and I think that they have to take a lot of credit for what happened with John too because they helped us make this decision for him. And I think it was a very stressful decision for them and they really were a great family to work with.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
Natalie Solimeo, PR CHOP
856-261-8090
Sign up for a free weekly e-mail on Medical Breakthroughs called
First to Know by clicking here.