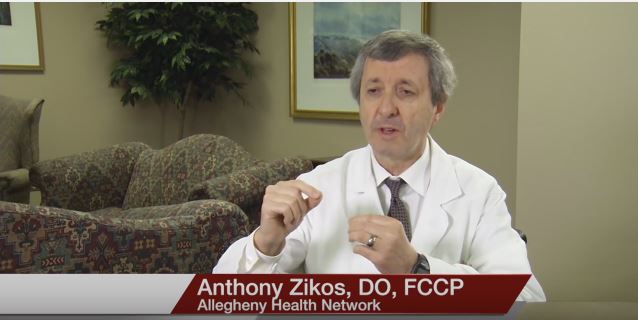
Anthony Zikos, DO, FCCP, Medical Director of the neuro-intensive care unit at Allegheny Health Network in Pittsburgh, Pennsylvania and a pulmonologist and intensivist, talks about a new groundbreaking procedure that will enhance the lives of asthma patients.
Interview conducted by Ivanhoe Broadcast News in September 2016.
In terms of asthma treatments has there prior to this procedure been anything nonmedical that has been able to treat people with severe asthma?
Dr. Zikos: Prior to this procedure the so called Bronchial Thermoplasty this was the only treatment we had as a medical/surgical treatment. This is the first surgical and the first invasive novel treatment that may to revolutionize the treatment of asthma.
What is this procedure called and kind of give me an overview.
Dr. Zikos: This procedure is called Bronchial Thermoplasty. Essentially it’s a procedure that uses heat radiofrequency. We perform this procedure utilizing a bronchoscope which is inserted in to the trachea with a complete examination of the entire lung. The Alair bronchial thermoplasty catheter is utilized via the bronchoscope to ablate the various regions of the lung as three separate procedures. We start with the right lower lobe, we do that as step one. Then, the second step is to move to the left lower lobe three weeks later, and then three weeks later we do the upper lobes; the right upper lobe and the left upper lobes are done last . By going in with the bronchoscope we use a catheter called the Alair catheter. This provides heat to about approximately sixty five degrees, Celcius, in thermal energy. The idea is to decrease the muscle mass of the endobronchial tree by applying heat or ablation. By decreasing the muscle mass you provide more room for air movement in the airways, recognizing that this is a simplistic explanation. There may be other mechanisms that are ongoing; however, you’re decreasing the muscle mass endobronchially, so you give more room for air movement. In fact, there is less spasm as it’s been shown now. But for the most part, it’s an anatomic problem because when you have a lot endobronchial muscle thickening, so called smooth airway muscle, and if you have an irritant which can be a virus, cold, or it could be an allergen, or many other things that can irritate the endobronchial tree. When you have this irritant it causes spasm. Now, if you decrease the muscle mass as this procedure does your chances of spasm are a lot less.
Is it a permanent fix?
Dr. Zikos: No, it’s not a permanent fix; however, four out of five patients get significant improvement. Some of the studies that have been published, at least a big study called the AIR2 trial, have shown that approximately twenty percent of these patients can come off steroids, with significant reduction of medications, significant reduction in hospital admissions, and eighty percent reduction of ER visits. There’s a dramatic improvement. But the most important thing that was measured in these studies was the quality of life. There was a drastic improvement in the quality of life.
How long will this procedure last, are you talking months, a couple of years?
Dr. Zikos: We have data up to five years that’s been published; this data of five years show that this is a lasting affect for at least five years and likely longer. But, the data we have so far at five years out appears to be equally effective and lasting
Can the procedure be repeated five, ten years down the road?
Dr. Zikos: No, the recommendation is not to repeat the procedure once it’s done. Because there is no way to know how much reduction of muscle you created, if you redo the procedure, there may be a danger of reducing the muscle too much and creating a problem. It’s not recommended to repeat the procedure, you only do it once.
What would be the options for the patients that undergo this BT down the road if they start having problems, is it back to medication, does it make the medication more effective?
Dr. Zikos: Less medication usually is what we’ve learned so far. From what’s been published, there’s usually less medication used, less asthma attacks, less emergency room visits, and less hospital admissions. When people have asthma attacks, and it’s been my experience -for the limited experience we have had now for the last couple of years, these folk’s attacks are not as severe. They’re able to get through much easier. One of my recent patients would say she would be at the doctor’s office thirty, forty times a year and now she had a cold the other day and she was able to get through it with no asthma attack and no ER visist. It all depends on the patient, but usually if they do get an asthma attack, the incidence is less severe, number one; and number two, usually it does not require a doctor’s visit.
You had mentioned that this is done in three steps three weeks apart, why is that?
Dr. Zikos: Because anytime we apply thermal energy it takes a while for the inflammation to subside. Keep in mind that we’re introducing radiofrequency heat. It’s like the cardiologist doing an ablation on the heart for atrial fibrillation. It’s the same idea only in the lung; except that we do anywhere from forty to eighty to ninety ablations. Therefore, the lung is irritated and in fact the first couple of days they can go in to bronchospasm. There can be a little bit of bronchial spasm, some coughing and there’s irritation. When you’re done, there are irritational effects from the procedure, so you need to give the lung a chance to settle so they can tolerate the next procedure.
Is this an outpatient procedure?
Dr. Zikos: It’s an outpatient procedure. They come in the morning, they get prepped. Usually we do a spirometry as a base line to see how their flow rates are; then once we’re satisfied with their flow rates and make sure they’re not having poorly controlled asthma. We check them over and make sure they’re doing well clinically. If they’re doing well then we proceed with the procedure. Then we watch them for approximately two to three hours after the procedure, and then once they’re stable they go home.
So in that day and back home?
Dr. Zikos: Right, the same day.
I guess you could consider this minimally invasive, there’s no cutting?
Dr. Zikos: There’s no cutting, correct. This is a minimally invasive procedure- correct.
There’s a special scope that goes down first?
Dr. Zikos: Correct. With the help of the anesthesiologist, we usually put these people to sleep; it’s much more comfortable, they’re more cooperative, they’re not coughing and we’re able to actually do more thermoplasty to more areas. If you’re coughing and the catheter moves, it technically makes it more difficult; so the anesthesiologist usually helps us and puts them to sleep and they’re very comfortable. Through the endotracheal tube, that the anesthesiologist has inserted, we always start with the right lung and we go to the right lower lobe and we start distally as far as we can go, as far as we can see the catheter and then every five millimeters we walk it back and we thermoplasty that area. Then we go to the different sub-segments and we try to accomplish as much as we can, as much as is visible we’re able to thermoplasty. The idea is that the more area you do, the better the results are, although we have no proof of that. But it would intuitively make sense the more of the lung that we thermoplasty the better of a chance that we are able to be successful.
With a camera on the scope, is that how you’re able to do it?
Dr. Zikos: There is a camera at the end of the scope and everything that we’re doing is visualized and we’re seeing where we’re going and we thermoplasty the area. So then, we do the visible distal airways first, and then gradually we move back. And I’ll show you on the model exactly how we start.
Was Jennifer McBride your patient?
Dr. Zikos: Yes.
Can you tell me a little bit about the difference you’ve seen in her, we’ll be speaking to her later today but you had mentioned quality of life, what kind of a difference is this really making for her?
Dr. Zikos: Jennifer had a poor quality of life. She couldn’t really do her housework, she couldn’t go up the one flight of steps, she was really miserable because every day she had to struggle. She told me she would go to the doctor’s thirty, forty times a year. Almost once a week she was at the doctor’s office, multiple admissions, multiple emergency room visits. Now, even in the short time of a couple months, to three months, none of that has occurred so far. She has done exceptionally well and she feels great. We have had other patients that they tell me they haven’t been able to do anything for a decade and now they’re able to ride their bike, they’re able to garden, they’re able to do other things that they were not able to do before; it has improved their quality of life, and in fact, not only did it improve it, but it probably enhanced it in many respects.
You had called this procedure groundbreaking, from your perspective can you tell me why?
Dr. Zikos: It’s the only surgical procedure so far. Many things have been tried in the past without success. But asthma is a complex disease, it’s a multifactorial disease and one procedure will not solve all the problems but this is really an adjunct. It’s going to be very helpful in managing especially these complicated patients; and remember, the patient who is a candidate for this. You’re talking about people who have poor quality of life, who are on moderate to high doses of steroids, and somebody who is on constant inhalers. Long-term, there are a lot of side effects with the steroids. Also, the thing that hasn’t been mentioned is the biologics. We use a lot of biologics many of these patients like Xolair. Now these are costly, and not only that, it’s a major commitment; the patient has to go once a week or every other week to the doctor’s office to get the shot. There are a couple of long-term problems that we don’t even know about. Nothing is perfect in medicine but you’ve got to weigh the good and the bad and I really like the benefits, they are much greater than the risks in doing this procedure in my opinion.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
Stephanie Waite
Media Relations
412-330-4434
Sign up for a free weekly e-mail on Medical Breakthroughs called First to Know by clicking here.