Ahmad Sedaghat, MD, PhD, Director of Rhinology, Allergy and Anterior Skull Base Surgery and Associate Professor of Otolaryngology at University of Cincinnati College of Medicine, talks about how more people are reporting problems with their sense of smell long after their COVID diagnosis.
Could you tell me first of all, a lot of our viewers probably have not heard that term. So, what is parosmia and what are people dealing with?
SEDAGHAT: Sure. Parosmia is a distortion of one’s sense of smell. So, things that you would smell and normally you would recognize them easily don’t smell like what they should.
Before COVID, how common was it?
SEDAGHAT: Uncommon. It could happen sporadically. Typically, it happens for the same reason during COVID and has happened during the pandemic for the same reason. It’s typically a byproduct of injury to one’s smell nerves.
Illness or a tumor? Would there be other reasons prior to COVID where people would have this happen?
SEDAGHAT: Sure. Anything again that could cause injury to one’s sense of smell and in particular injury to the smell nerves, the olfactory nerves that live at the top of the nose and the top of the nasal cavity, could cause parosmia.
You said fairly rare prior to COVID, so tell me what’s happening now.
SEDAGHAT: We know that COVID-19 is an incredibly prevalent infection that’s going around. In particular, the virus that causes COVID-19 seems to have a predilection for infecting the cells that live near the smell nerves and subsequently causing secondary injury or maybe even death of the smell nerves. So even though we know that smell loss can occur secondarily to viral infections, in the past it was actually quite rare. It seems to be very common with the particular virus that causes COVID-19, which is why we’re seeing so many patients that are experiencing smell loss, and then as a secondary byproduct, they’re experiencing this parosmia.
About how long after COVID could this develop?
SEDAGHAT: So, it can happen any time during the COVID-19 infection. More frequently, it happens afterwards, typically around one to four months after the initial infection.
So, you’re getting better, you’re feeling better. And then what happens?
SEDAGHAT: First, it’s important to understand that this is a secondary effect of injury to the smell nerves. So, these are patients who experienced smell loss during COVID-19. What typically happens is they feel like their sense of smell has either completely recovered or is recovering. Then one to a few months later, they may start to notice that things don’t smell like they used to. In fact, the changes to the sense of smell are typically quite bothersome. They can be things like gasoline, smoke, fire, rotten food, rotten flesh. Those are typically the smells that these patients are sensing when they might smell their morning coffee, their dinner. So, this is typically what happens.
Is this also affecting sense of taste?
SEDAGHAT: Sure. But we have to be careful in terms of how we refer to taste. Taste itself is your ability to sense sweet, sour, bitter, salty, savory. We typically use the word taste to refer actually more to flavor, which is an integration of multiple senses, your ability to taste those senses or those different tastes that I mentioned before. It integrates your sense of smell. It actually even integrates your ability to sense textures, acidity, heat of food. All of those senses coming together forms your ability to sense flavor of food. I always think about flavor of food as something analogous to the color in a picture. You can tell what a picture shows without color, but it’s just not quite the same as having the color there. That’s sort of the flavor of food. So, when your sense of smell is either gone or diminished or altered, it certainly can affect flavor of food.
Is this a permanent condition?
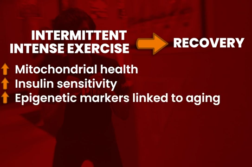
SEDAGHAT: We don’t think so. In fact, quite the opposite. We think that parosmia is a positive prognostic indicator of recovery in one’s sense of smell. What’s interesting is that people are generally not very good judges of how good or bad their sense of smell may be. So, when they have that smell loss or injury to their sense of smell during COVID-19, and they feel like they’ve completely recovered, in pretty much all of these cases they actually have not completely recovered. It’s just that they are recovering and things are getting better. There’s still injury there. There’s still healing going on. And we think what’s happening during parosmia is that as those smell nerves regenerate and regrow, which is actually a really nice thing about our olfactory system, there are plenty of stem cells that live up there and can regenerate anything that essentially dies. So as these smell nerves start to regenerate, we think that some of them may rewire incorrectly, and that’s what causes the parosmia.
Is there a treatment? I mean, is there anything you can do for patients while we’re waiting for that regeneration to happen?
SEDAGHAT: So, the best evidence-based treatment for smell loss, first of all, is something called olfactory training, which has been described as essentially practicing smelling concentrated odors to essentially stimulate your smell nerves. That may help either through the direct stimulation, getting them to grow or even thinking about what those smells are like reactivating your olfactory system. I still suggest that for our patients who have parosmia for a couple of reasons. First, we know that the parosmia occurs as a matter of recovery. It happens during the course of recovery. So, we still want to treat these patients as individuals who have injury to their sense of smell, and we want it to recover. The second part is that your sense of smell actually has multiple components to it. We typically focus on our ability to sense odors. Your sense of smell is actually more than just your ability to detect the signal. It’s detecting the signal, but it’s also having that signal routed to the right memory centers in your brain so you remember what things smell like. That’s actually what we think is happening in parosmia with that miswiring where you sense the signal but those signals are not getting sent to the right place. In fact, they’re getting sent to places that get you to remember foul odors, and we think there’s reasons for that as well. When I have patients do this olfactory training after or during when they’re experiencing parosmia, I advise them not only to practice the smelling and getting that signal up to their smell nerves, those recovering smell nerves to stimulate them to continue to grow, but also advise them to think about what those odors smelled like. What did they smell like? Because that activates those memory centers. It activates the smell nerves, and nerves that get activated together at the same time tend to want to connect with one another. Beyond just the practice of the olfactory training and doing this a couple of times a day, I always make the analogy and refer to it as physical therapy for smell nerves. So, it’s done very systematically. You do it a couple of times a day. Particularly you do it for certain times for each odor. I actually advise patients to do this as they go through their day-to-day life. In particular, focus on those things that are really bothering them rather than staying away because you really need to get those smell nerves to wire to the right place.
How long does it take to recover? Does it depend?
SEDAGHAT: We don’t know. This is still a matter of study. We’ve seen patients where it gradually starts to diminish after a few months, where it can go away after a few months, but we have patients also who are still a few months into this who still have it.
If the physical therapy isn’t working, is there a medical fix or a surgical fix?
SEDAGHAT: Not that we know of right now. There are different medical and typically topical therapies that are currently being studied right now but none that I would say are strongly supported by evidence.
Anything I didn’t ask you that you would want to make sure people know?
SEDAGHAT: Well, sometimes I get asked why? Why are the parosmias so foul? Why is it always foul-smelling things? It’s never patients ever come in saying, gosh. Everything smells like roses. It’s always smells like trash or fire or smoke or cigarette smoke. We think the reason for that is that our physiology is programmed so that if this miswiring occurs, we err towards the side of smelling danger signals. At the dawn of man when our survival depended on being able to smell dangerous signals, it was important that if you experienced injury to your smell nerves, which we actually think happens pretty commonly, which is why we have so many stem cells that live in that olfactory epithelium, if that happened early in the course of our species, we would want our physiology to err on the side of smelling those dangerous signals rather than roses or something not necessarily critical to survival.
I know you said that you’ve seen tons of patients. Could you give me a guestimate of how much of a percentage it’s increased?
SEDAGHAT: Hard to tell you exactly how much it’s increased. I mean, it’s dramatically increased since the pandemic. What I can tell you is that some of the early studies on this, and I would roughly and approximately confirm it in my own practice, is that anywhere from about 15 to in one study, up to 50 percent of patients who experience smell loss during COVID-19 may experience parosmia at some point afterwards.
Interview conducted by Ivanhoe Broadcast News.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
Bill Bangert
Sign up for a free weekly e-mail on Medical Breakthroughs called First to Know by clicking here