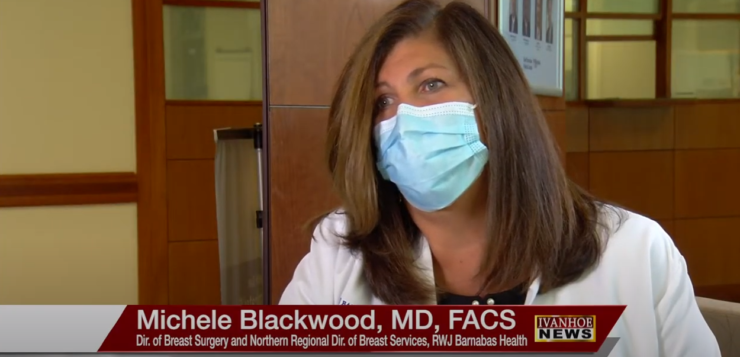
Michele Blackwood, MD, FACS, chief of breast surgery at Rutgers Cancer Institute of New Jersey, system wide director of breast surgery at Northern Regional director of breast services for RWJ Barnabas Health, and medical director at the Center for Breast Health & Disease Management at Barnabas Health Ambulatory Care Center, talks about a new method for ensuring all cancerous and pre-cancerous cells are removed during a lumpectomy.
So, the lumpectomy as a treatment. Can you, just for our viewers who may not be familiar, describe what that is and how common it is?
Dr. Blackwood: Sure. Lumpectomy is a very nice treatment option for breast cancer. It requires taking out the tumor itself with some surrounding tissue, and that’s called a margin. It’s very important to get the whole tumor out, obviously, and also to have a nice piece of tissue around it, but not too much because you want the breast to look and feel like a breast when you’re done. It’s a nice option. The other option, of course, would be mastectomy, where you take all the breast tissue out, usually reconstruct it, but the reality is that over 70 percent of our patients choose lumpectomy with radiation.
You said it was 70% who choose lumpectomy. What are some of the reasons why they would choose the lumpectomy?
Dr. Blackwood: It’s interesting. People choose lumpectomy because, A, they get to keep their breast. B, they look and feel like themselves. C, it’s much less surgery. D, they have less anesthetic, a much faster recovery. And in this day and age, with the issues with jobs, they get back to their job faster.
With lumpectomy, how successful a treatment is it for breast cancer?
Dr. Blackwood: Lumpectomy and radiation is equal to mastectomy in survival. Most people don’t know that. So, they’re pretty surprised that they could take a minimal operation and get rid of their breast cancer and have equal survival to the woman who chose mastectomy. The difference is that, with the lumpectomy, you need to have radiation post-operatively. And the other thing is the chance of recurrence in the breast is slightly higher. It doesn’t mean your survival is impacted upon, it just means that you might have a chance of growing another cancer in that breast at some point in your lifetime.
I want to talk to you a little bit about a second surgeries or re-excision. Under what circumstances does that need to happen?
Dr. Blackwood: So, when I perform a lumpectomy, it’s very important to get the whole tumor out and a margin of tissue around it that’s negative for tumor. Because in our minds that means we got the entire tumor out. Tumor’s sometimes are mixed. Sometimes they have invasive cancer and pre-cancer. And the issue is the pre-cancer particularly can be on the outside of the tumor. You don’t feel it. You can’t see it with the naked eye. So after I get the tumor out, I put six different colored inks on that specimen, I mark it with these charms that tell me which margins are which, and then I take an X-ray of it right in the operating room. And that X-ray is done with the Kubtec and it looks beautiful. And then I can tell how close each margin is, I can actually tell if I’ve gotten the specimen that I need out – because many of these cancers we can’t feel. So, you’re using radiology guidance to find these, and it’s very reassuring when you’ve gotten the whole tumor out.
You said it looks beautiful and you talked about – that you put the dye and you marked it. What does it look like for you?
Dr. Blackwood: So particularly with MOZART Kubtec we’re able to see a photograph of the specimen itself . So, I can see all the different color inks I put on and the charms and then there’s a very fascinating piece to it where the machine actually goes through the piece of tissue in small increments, and I use it to measure the distance from the margin that I see as negative down to where the tumor is.
I know it sounds like a simple question, but what is the benefit for you, first of all, as a surgeon for having this tool at your disposal?
Dr. Blackwood: There’s a huge benefit to not taking a patient back to the operating room at any time. So, the complications that can occur with a lumpectomy include the fact that sometimes the margin is positive meaning the edge of the tissue has cancer cells in it. We never want to do that. We never want to leave cancer cells behind. So, if I can take an X-ray in the operating room I can assess radiographically if I’m close or not. If that pathology comes back a week later and tells me that there’re cancer cells at the edge I have to calm my patient and tell her that we really need and should go back to the operating room to clean that edge up. So the benefits to having the Mozart KUBTEC in the operating room is that I get to assess that I took out the right tumor, that I have all the calcifications or the little white dots on the mammogram that I was after, I get to see how far the tumor is from the edge of my specimen and then I also get to assess it radiographically to see how far it is from all the edges. Because the picture generated by the KUBTEC is fascinating. It gives us slices through the specimen so we can see and assess how far the tumor is from the edge.
What would you have to do before? It wasn’t in real time before. Was there a process after you were done?
Dr. Blackwood: It’s hard to even think about because I don’t know what to think about it. Before when we took the tumor out, we still inked it the same way. We still put the same charms on. But in our surgery center we would have to send the specimen down to the breast center which is on a different floor. Have to take an elevator. There has to be someone from security. The team in the operating room is waiting. And we’re just sitting there waiting for the information for the radiologist to call us and tell us what she’s seen. The problem with that is obvious right? You can’t see it. You can’t assess it yourself. I know where I was in the breast and how I took it out and how I inked it. And she can only tell me, “oh, yes, it looks a little close to one of the margins. I’m not sure which.” Or she can say, “yes, you got it.” Or sometimes it just took a long time because she was in the middle of another procedure and we’re sitting in the operating room for upward sometimes of 45 minutes.
Just waiting for that confirmation?
Dr. Blackwood: Just waiting for the confirmation. And if you’re waiting for the confirmation, you don’t want to leave the patient on the operating table too long. This is real time. I no longer have to wait 45 minutes. Literally while I am finishing the operation, the nurse is taking the picture. And I end up being able to assess it right in the operating room.
What would you want patients to know about this extra tool that you have with the Mozart?
Dr. Blackwood: I actually think now in 2020 that it’s very important to ask your surgeon whether this is available for them in the operating room because the shorter you’re on the operating room table the better it is from a bleeding risk, an anesthetic risk, an infection risk and, quite frankly, a blood clot risk. So, you want to know that your surgeon is being as precise as possible. I personally feel now in 2020 this should be standard of care.
Is there anything I didn’t ask you that you would want people to know?
Dr. Blackwood: That’s a good question. I do think it’s important that patients understand how much work we go to to keep that specimen oncologically pristine, meaning, it’s not just like we go in and take out a lump and you’re done. There’s a science to it. There’s a technique to it. These details are very important. And when I see a patient for a second opinion that hasn’t had this I always know because when patients get positive margins, they want to get second opinions.
And about how many have you done? How long have you had the tools available to you?
Dr. Blackwood: We’ve had a KUBTEC for, to be honest with you I was at year five. I’ve been here 12 years and for five years I begged and borrowed for it. And finally at the fifth year I’m upstairs doing a case. And I had to wait in line because another breast surgeon who doesn’t come here was using it for the first time. I was like you’re kidding.
And you were the one begging for it?
Dr. Blackwood: And I was begging for it. But they didn’t have the Mozart till recently. We had a KUBTEC tech here since for seven, eight years now. We just updated it this last December.
And any estimate of how many cases you’ve done in since?
Dr. Blackwood: So, I’m one of four surgeons here and we do about together. So, I do about 300. She does about 250. We as a group have probably done close to a thousand cases on it. It’s not just cancer cases you use it for by the way. There are a couple of other uses for it. And that would be something to tell patients. So, if a patient had an enlarged lymph node and she received chemotherapy, that’s called neoadjuvant chemotherapy. So, we have biopsied the lymph node ahead of the chemo. We biopsy the tumor and the lymph nodes. So, a clip is put in the lymph node. And the clip is put in the tumor. And after chemotherapy, things get a little sticky sometimes inside. But when I get the special lymph node out that has the clip in it. It’s very important to get that lymph node out. And I get an X-ray of that lymph node as well.
And you can do that with a?
Dr. Blackwood: I do it with the KUBTEC. And the other thing that is important is that we don’t use a localization. So either we put a wire in or a clip or something and tells us where that little spot is, say the spot is not that little or it changed in shape since we examined the patient, and we take it out without any guidance, then you can also get a picture of the specimen of the lump itself.
And the only other question I have for you doctor is I just have to ask about just full disclosure. Do you have any ties to the company? Do you speak for the company?
Dr. Blackwood: No. I negotiated the contract. We’ve had KUBTEC in this institution for years and years so.
Interview conducted by Ivanhoe Broadcast News.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
John Leach
Sign up for a free weekly e-mail on Medical Breakthroughs called First to Know by clicking here