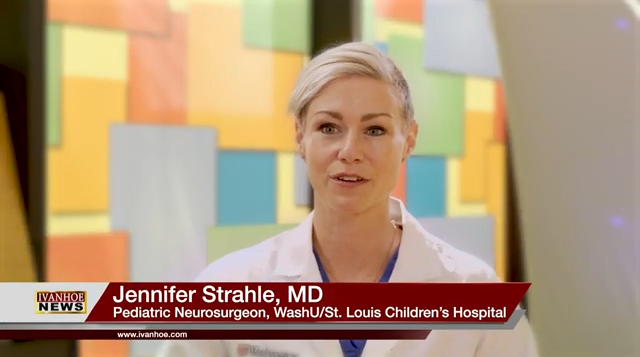
Washington University and St. Louis Children’s Hospital pediatric neurosurgeon Dr. Jennifer Strahle and neonatal & pediatric neurologist Dr. Lindsey Peglar Marsala talk about removing a tumor from an infant’s brain.
Interview conducted by Ivanhoe Broadcast News in 2023.
Can you tell me about how you found baby Elizabeth’s brain tumor?
Strahle: Elizabeth’s story is quite unique in that her tumor was found in utero. We detected it before she was even born.
How far along was she?
Strahle: I first met them when her mother was about 36 weeks gestation.
And it’s a special brain tumor. What kind?
Strahle: Yes. She has something called a teratoma, which is a rare tumor when it occurs in the brain. It’s a very rare tumor type.
Are they the ones that can have teeth and hair?
Strahle: Exactly. The definition of a teratoma is a tumor that has tissues that contain multiple types of tissues. It can have hair and teeth than tissues from all over.
How big was this tumor?
Strahle: As far as tumors go, this was an extremely large tumor.
Where was her tumor?
Strahle: The tumor was right in the center of her brain.
Did that make it trickier?
Strahle: Yes, it made it very tricky. What was difficult about Elizabeth’s case is that she was so small. When children present with brain tumors that are a little bit older, let’s say over a year of age, they’re old enough and large enough that they can tolerate surgery to take the tumor out. In Elizabeth’s case, she was very small, and little babies do not have a lot of blood volume. We had to be very careful in terms of the timing of when we take something out.
And for Elizabeth, this was pretty miraculous really because a lot of times the babies who are born with this, especially where it was in her brain, might not survive?
Strahle: Correct. When you take teratomas as a whole, we’ll sometimes see small teratomas on the periphery of the head or other parts of the body. They can be more straightforward to manage. Her teratoma or her brain tumor was extremely large and was difficult to get to and also was associated with very critical parts of the brain that control a number of different functions.
How was it impacted?
Strahle: It impacted her. When she was born, she did have seizures which we were able to manage with medications pretty easily. The tumor was associated with areas that control movement or motor function. That was probably the biggest area that we saw in effect.
Was the tumor responsible in any way for the cerebral palsy?
Strahle: I think ultimately the tumor and the way that her brain develops. Because the tumor occurred so early in development, even before she was born, some parts of the brain did not form as they normally would because there was a large tumor present.
How long did you have to wait? Was she born early and how long did you have to wait until surgery?
Strahle: She was born around term meaning she was not a preterm infant. When she was born, she had something called hydrocephalus. That’s when there’s fluid accumulation in the brain. The reason she had that is that the large tumor was blocking off the fluid flow. There was an accumulation of fluid. Early on she had a shunt. She had a procedure to drain the fluid, and then we also had to determine what we were dealing with. When she was born, we did not know the diagnosis. She had a biopsy, then once we figured out what we were dealing with, we then planned on doing surgery when she was older, between four and eight months of age.
Is that one of the youngest babies that you’ve ever operated on for this type of tumor?
Strahle: I think for the size of this tumor and to be able to take the tumor out in its entirety, yes. She was one of our youngest patients to have such a large tumor completely resected.
Can you give me an idea of the size?
Strahle: It was bigger than an apple. It was more of a grapefruit size. So Elizabeth’s tumor was about the size of a grapefruit.
Had you ever seen anyone that large in such a small?
Strahle: In such a young patient, no.
What was the recovery like?
Strahle: Elizabeth did remarkably well throughout every stage of the process. The tumor was a little bit challenging because it was so diverse in the types of tissues that it had or the types of cells. The tumor itself was making cysts, which are fluid-filled pockets. Before we were able to take out the tumor, we had to perform surgery to drain those cysts and get her to a point where she was old enough. When we took the tumor out, she did very well. We were able to take it out in one procedure, and her recovery was really quite remarkable. She’s done amazing.
Will the brain fill in or has it already learned to rewrite around that or what?
Strahle: Yes. Afterward, because the tumor was so large, she had a lot of extra fluid filling that space. That was another challenge in her care and we needed to make sure that that extra fluid was not causing her additional problems. Over the course of the last year and a half, her brain has continued to grow and her head size has stabilized. Over time, everything is filling in as her brain grows.
Is there a lot of hope for this little girl?
Strahle: Yes, tons of hope. Every time I see her in the clinic, I am amazed at the progress she’s making, and how she’s really near the level of her peers for her age. Even in some cases, she’s more advanced than other kids her age that I see, particularly in terms of cognition and what she’s able to do.
If this would have happened 10 years ago, would the outcome have been different?
Strahle: Possibly. The success of her case was the result of a large multi-disciplinary team, where we were really able to have a lot of different areas of expertise coming together to take care of her. When you look at large teratomas in the brain that are diagnosed before birth, there really are not very many reports in the literature of successful surgery.
Tell me when you first met baby Elizabeth.
Peglar Marsala: I met her mom and her grandparents around when her mom was about 36 weeks pregnant because they had had an ultrasound at the very end of her pregnancy when everything had been going well and then they were worried that they had found a tumor or a brain tumor in Elizabeth.
Had you ever seen anything like that before?
Peglar Marsala: This is something that is really, really rare, especially in a baby that hasn’t been born yet. This is one of the first cases that I had seen.
What would the diagnosis for Elizabeth be after she’s born?
Peglar Marsala: After she was born we didn’t really know exactly what this was. Her original diagnosis was she had a brain tumor and we had to figure out exactly what it was and what would be the best course of treatment for her.
What was your journey with Elizabeth then?
Peglar Marsala: When Elizabeth was born, we were really counseling her parents and her grandparents about the next steps and what was going to come in her care. We had to figure out what was going on first and then what would be the best course of treatment for her. Then after that, managing any complications that came up with her numerous surgeries and other things.
Now, at that point, did you know that she had cerebral palsy?
Peglar Marsala: At that point, no we didn’t because cerebral palsy shows up with time, really. It took us a couple of months to years to figure out that she did have cerebral palsy. Then when she did giving her a diagnosis as soon as possible to help her get the therapies and the support that she needed to help her achieve everything that she can.
Did it take a large team to get Elizabeth where she is today?
Peglar Marsala: Absolutely. Really, the credit for how well she’s doing today comes from her multi-disciplinary team both while she was an inpatient in the hospital and while she was an outpatient as well. Then also from her family who has been so supportive every step of the way her mother and her grandparents.
Tell me about what happened after the surgery for Elizabeth?
Peglar Marsala: Elizabeth had some complications that can come with complex brain surgery. She had seizures which were controlled with medications, and she’s been doing very well from that standpoint since then.
Does she have any more seizures?
Peglar Marsala: She has not had any more seizures since her immediate surgeries.
Is that medication something that she may have to stay on for life or will you wean her off of it and see if with her brain developing if that goes away?
Peglar Marsala: Yeah, it’s really exciting because we’re going to talk about weaning off of her medications really slowly. It’s fun to be able to have those good conversations with families too, about how well she’s doing and all the good steps forward we can make. Not just all the critical things and the scary things that come with it. We don’t know what exactly what’s going on and we need to figure it out.
After surgery, what were some of her complications other than the seizures?
Peglar Marsala: She did have problems moving the right side of her body and that’s where her diagnosis of cerebral palsy comes from too.
It’s only right-side cerebral palsy? Is that unusual?
Peglar Marsala: No, but that side of her body has the most trouble with movement and muscle tone. On the left side of her body, she can move easier than her right, but she still uses both sides.
How will that impact her as she grows? Is that something that she’ll be able to do with therapy and live a normal life?
Peglar Marsala: Absolutely. That’s one of the best things about her story is that she had really good therapy support from the beginning. She’s made great strides and is able to walk independently and use those sides and she’s making great developmental strides.
I just can’t imagine what the feeling is every time you see her.
Peglar Marsala: It always makes me so happy to walk in because she’s always smiling and her family is wonderful and it’s great to be able to focus on all the great things she’s doing now instead.
What will be her challenges moving forward?
Peglar Marsala: Her biggest challenge is going to be her cerebral palsy, but she’s really overcome that very well. She’ll probably always have issues with that right side of her body and the way she’s able to move it, but she’s overcome that and she’s able to work around that.
Should she be able to live a normal life mentally? Is she going to be with the other second graders and third graders?
Peglar Marsala: I have high hopes for her and she’s doing really well from that cognitive standpoint at this time. She has great potential.
Do you feel like there was anything when Elizabeth first came here, that for her transferred to the fetal care center, or anything you feel would be helpful?
Peglar Marsala: I think one of the biggest challenges at the beginning of her story was the unknowns because we didn’t quite know what her tumor was, what it would do, or what she would be like after all of her complex procedures. But now it’s more of celebrating what she’s doing now and looking backward at where she’s been and all the steps that she’s making.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
Judy Martin Finch Rachel Yann
martinju@wustl.edu Rachel.yann@bjc.org
Sign up for a free weekly e-mail on Medical Breakthroughs called First to Know by clicking here