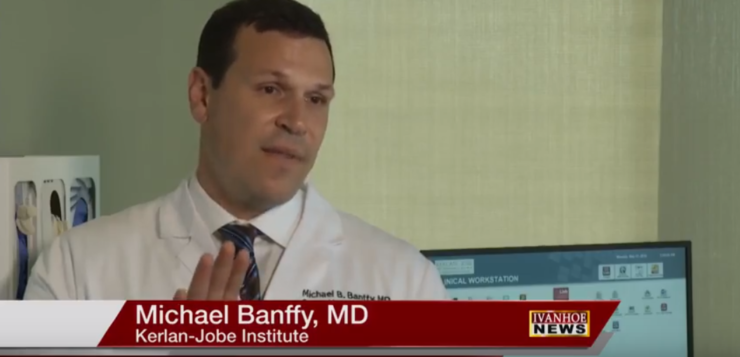
Michael Banffy, MD, Orthopedic Sports Medicine and Joint Preservation at Kerlan-Jobe Institute talks about using a patient’s own cells for their knee replacement.
Interview conducted by Ivanhoe Broadcast News in April 2018.
Tell us about MACI, it sounds like a pretty good option for knee replacement. How does it work?
Dr. Banffy: I wouldn’t say that MACI is an option for knee replacement. Knee replacement is also a resurfacing, but it’s done with metal and plastic. MACI is a resurfacing and we’re really trying to restore the biological surface or the cartilage surface of the knee. In someone that’s a candidate for a knee replacement, there would be diffuse cartilage damage. When people have potholes in their cartilage – that’s really where the MACI will fit in. There’s lots of different ways to fix these potholes, but MACI is really the only way to do it where you’re using a patient’s own cells, own cartilage cells to fill those defects in.
It’s growing stem cells, is that right?
Dr. Banffy: It’s not really stem cells. It’s growing the cells that already exists. It’s a two-part procedure where we go in first with an arthroscope. With the arthroscopy we’re able to really evaluate that pothole that’s in the knee. We’re able to size it and we’re able to see if they’re a candidate for MACI. Once we have that determination we’re able to take a biopsy. We take a little piece of cartilage from the knee in a non-weight-bearing surface, a place they’re not going to miss it. Send that into the lab and it’s those cells, those actual cartilage cells, so these are after the stem cell stage. They’ve already found their focus on how they’re going to mature and they replicate those cells. They then embed them on to a membrane which is called the matrix and that’s what we put back in the knee.
The matrix goes on the pothole.
Dr. Banffy: Exactly. The matrix has the cells embedded on it and I’ll just take those cells and pop it right over the pothole.
How do they grow those cells in the lab?
Dr. Banffy: It’s a cell culture. I take a biopsy of the cartilage which is grossly matrix that surround these chondrocytes which are the cartilage cells. When I send those in they break that matrix down just to get those cells. And then they culture those cells through methods that are above my head. And then they’re able to replicate that then put that on to the membrane.
So during the main surgery you cut it and make it perfect and then stick it in there and just let it do its thing?
Dr. Banffy: I will define the area of the cartilage defect, either in an open or arthroscopic procedure. Once that’s defined I can take a template, typically some sort of sterile foil and then from that sterile foil I can cut the actual membrane to size and then glue that in with something called fibrin glue.
How long does it take for the cells to start doing their thing?
Dr. Banffy: It’s almost immediate. Within sixty minutes there are cells that have already adhered down to the bone below. It occurs very quickly. But the rehabilitation process does take a while and that’s because not only you are trying to get the cells that are already on membrane to adhere but you want them to grow. And you want them to really fill in that defect. So that takes some time.
Right. A year?
Dr. Banffy: A year before your back to full activities. You probably have a good seventy five percent fill within about six months.
So how does this compare to the other similar techniques that are out there, if there is anything even similar?
Dr. Banffy: Well, there’s a lot of different techniques. One thing is called micro fracture where you poke holes in to the bone, getting the bone to bleed. Maybe some stem cells that will turn into cartilage cells will fill that in. That’s good in really small defects, but nothing that’s bigger than one cm. There’s some donor cartilage that’s available out there, it works – but the data is not as robust as it is for MACI which has been done in Europe for the last fifteen years and patients like utilizing their own cells. I think that because of that, MACI offers a real potential for the patients to maintain “whole”. And then there’s also something called osteochondral allograft where you’ll get a donor that is a knee that looks identical to the knee of the patients, has the same curvature of radius as well as the sides. And if there’s a defect that is really large that may be out of the realm of using MACI for example, or if it’s in a particular area, or if there is a lot of bone damage because the MACI doesn’t necessary account for the bone. You have to do something to the bone’s separate to it. This osteochondral allograft can account for all of that so you would take a plug from one and put it in the other it.
So far, what is your reaction to the results from MACI operations that you’ve done?
Dr. Banffy: They are fantastic, prior to MACI we used to call it ACI. MACI stands for matrix autologous chondrocyte implantation. ACI was just autologous chondrocyte implantation. It is the same procedure, where we take out the cells and grow them. They would send into a vile and we’d put them into the pothole and then cover it with a membrane and sew that in. Those results were great and then MACI has furthered this I think, I wouldn’t say they made the results better. They maintain the same results, but they made the surgery a lot simpler, less invasive and really more accessible for areas they knew that ACI was not able to do. I recently or just referred to non-contained defects, areas that pothole may be a little shallow on one side. Because you couldn’t sew the previous membrane in, you couldn’t use that old technique now that were gluing the membrane in. It works really well.
Karen is a runner, she can’t wait to get back out and run if that’s possible. Do you see that as being in her future?
Dr. Banffy: That’s the reason we did the surgery we did. I think her other option was a partial knee replacement potentially and her running is not just a normal running. This is hundreds of miles of running. Doing an osteotomy for her with the MACI was really the best way to restore her joints. I think that the hardest thing for Karen is really trying to go through this year of recovery. Especially since I work with her in the same building, it’s hard for me too.
She doesn’t think she can do the distance again but is she realistic to think that she can try it again?
Dr. Banffy: Currently, I understand she just walked for nine, ten miles in Paris. I believe that she’s on nine months out at this point, so that’s pretty phenomenal.
What haven’t I asked you about the procedure that you would like to include in the story?
Dr. Banffy: I think that the areas that MACI are really effective are areas that are very undulating. There really is no alternative for cartilage restoration underneath the knee cap or on what we call the trochlear groove, that’s really good for this technique.
How about the future: hips maybe, ankles, elbows, shoulders?
Dr. Banffy: Well cartilage problems exist in all those joints and so that definitely is the frontier. We need to figure out with regard to the biopsy either can we take a biopsy from the knee and use it in those other joints. Does it have to be the cartilage from those joints? Accessibility to those joints, really the techniques with arthroscopy are going to be very important. So I think that is definitely in the future something that I’m very interested in.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
Scott Stachowiak, PR
646-942-5630
Scott.Stachowiak@russopartnersllc.com
Sign up for a free weekly e-mail on Medical Breakthroughs called
First to Know by clicking here.