Varun Puri, M.D., MSCI, a cardiothoracic surgeon at Washington University School of Medicine in St. Louis talks about a new device that is saving the lives of people who need a lung transplant.
Interview conducted by Ivanhoe Broadcast News in April 2016.
I’ll start by asking you about lung transplantation. How desperate is the need right now?
Dr. Puri: As a matter of fact at one point in time we have several thousand people on a lung transplant waitlist. Every year the number of patients that get transplanted is about two thirds or less than two thirds of the people who need lung transplantation during that period of time. Therefore not only do we have patients who continue to have a low quality of life because of lung failure on a lung transplant waitlist but a certain percentage of them actually end up dying on the waitlist.
Why is it so difficult?
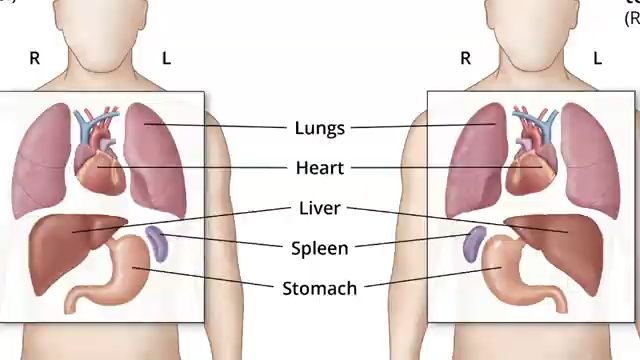
Dr. Puri: The lung is a difficult organ specifically because the donor situation is not conducive for lung transplantation. When you look at one hundred brain dead donors, which is the most common brain-donor pool that we have, only about twenty to twenty five percent of them end up being eligible to give lungs for transplantation, which is much lower than for any other solid organ in the body. Therefore there’s a perpetual shortage of donors compared to the recipient pool or patients waiting for transplantation In addition the lungs unfortunately happen to be such organs that they have amongst the highest short and long-term rejection rate after transplantation which further complicates the problem.
I wanted to ask you a little bit about the Ex Vivo, in what ways does this help in what you do with transplantations?
Dr. Puri: Ex Vivo lung perfusion technology has a twofold impact on lung transplantation. The first is that it allows us to use or access what we can call as marginal lungs for transplantations. Of the seventy five percent or so lungs that we end up not using there’s a certain proportion that end up being just below our strict cutoffs for using lungs for lung transplantation. It is that pool of lungs that you’re able to access on Ex Vivo perfusion technology. Other benefits of this technology are that there is a possibility that we’re able to improve the quality of some of these lungs to the point that they come above our strict thresholds and become usable for transplantation.
Can you give me an example on what kind of things are going on with the lungs that makes them not eligible?
Dr. Puri: The most common reasons for lungs not being suitable for transplantation are one, infection that is pneumonia within the lungs. If for a variety of reasons there’s inflammation within the lungs and the most common response of the lungs to inflammation is that they get, edematous or in a matter of speaking waterlogged. Waterlogged lungs are not only inadequate for good oxygenation or gas exchange that means they function poorly, they in themselves become a liability for the patients that they’re in.
How could the Ex Vivo help? You said it would help improve the quality of lungs. By what percentage does it help if you are able to use it?
Dr. Puri: There is no way to really answer that question in terms of absolute numbers because the technology is so new. The application is also very limited. Right now it’s currently still on trial at a number of institutions in the country. One can’t give you a hard percentage of the increases in the number of lung transplants that are performed because of Ex Vivo lung perfusion but my estimate is somewhere between the ten to twenty percentage range increase in the number transplants due to this technology. Also the way Ex Vivo lung perfusion helps in possibly improving the quality of lung is that there is a propriety solution that runs through the blood vessels of the lungs, which contains a number of nutrient factors has the ability to actually pull water out of the lungs and decrease the water logging or edema in the lungs thereby improving their function.
Could you talk a little bit to me about Michelle’s case?
Dr. Puri: Michelle suffers from a disease called emphysema. Her quality of life is impacted to such a degree by emphysema or was impacted to such a degree by emphysema that she had difficulty with activities of daily living. These activities included walking across the room or brushing her teeth or putting her clothes on. These activities would make her significantly short of breath. Also these not only limit her daily activities it also decreases her interaction with people that are around her. That is just from a layman’s perspective. From a medical perspective she had what was called end-stage lung disease or end-stage pulmonary failure from emphysema.
What were her options in terms of treatment at that point?
Dr. Puri: Realistically speaking she was maximally managed with medications. No more medications would improve her breathing at that point in time and her only option was lung transplantation for improving the quality of life and her breathing.
When you say end stage what kind of a timeframe was she looking at?
Dr. Puri: It’s somewhat hard to put a timeframe on patients with end stage lung disease. There are two varieties of end stage lung disease; people with emphysema and people with other conditions like pulmonary fibrosis. Often times it’s the length of life from lung transplantation is not improved by much. It’s the quality of life that you have in patients with emphysema which is the great benefit in that patient population. For other end stage lung diseases like pulmonary fibrosis, lung transplantation improves both lengths of life as well as quality of life.
Can you tell me how the Ex Vivo played a factor in her survival?
Dr. Puri: Michelle in her blood stream had certain specific factors called antibodies which would make her an unsuitable recipient for the vast majority of donors out there. As a matter of fact more than ninety five percent of potential donors would not be able to provide organs for Michelle because of these pre-existing factors or antibodies in her blood stream. Therefore it was quite fortunate that we found a donor that was marginal, that was just below our threshold for utilizing for standard lung transplantation and who did not carry the specific antibodies that would react with Michelle and would make her reject those lungs.
The lungs you said were just below normal so what were you able to do?
Dr. Puri: What we were able to do was retrieve these organs from the donor and place them on the Ex Vivo circuit thereby both accessing the quality of the lungs over the next four to six hours as well as by running the fluid through the lungs, through the blood vessels of the lungs, trying to decrease the waterlog in the lungs to improve their quality. With these efforts the lungs actually became suitable for transplantation and we were able to use them clinically for Michelle.
Had she not gotten that transplant, those lungs that went through the Ex Vivo process what would have been her options?
Dr. Puri: Really no other options except lung transplantation for her. It’s highly unlikely she would have received transplantation even today many months after her transplant.
In your mind this saved her life?
Dr. Puri: Absolutely.
Talk to me about how she’s doing now.
Dr. Puri: Michelle is doing great. We saw her a couple of weeks ago, she is excited every day to be able to do things that she’s not been able to do for many years. She actually takes care of family members and grandkids. When even a few months ago all she was able to do was just sit and breathe with oxygen.
How often will you check up and how are her lungs functioning?
- Puri: Her lungs are functioning quite well. She continues to be on room air, she’s not requiring any oxygen. Her quality of life is much improved and she is in a continuous surveillance program where she is checked every few weeks for the first many months and then every few months for a very long time. Hopefully for her, it’ll be a very long time.
Is that a permanent improvement to those lungs or will lung function decrease?
Dr. Puri: The most important long-term problem after lung transplantation is chronic rejection. That unfortunately happens at a rate of about ten to fifteen percent a year long-term after lung transplantation. That’s not something that any current technology has ability to diminish.
But in terms of the lungs will they continue to function at this level?
Dr. Puri: If there is no chronic rejection the lungs should continue to work well for her. If however any patient after lung transplantation develops chronic rejection the function of the lungs does diminish.
What becomes the option of another transplant?
Dr. Puri: Another transplant becomes an option at that point in time however it’s not something which is commonly performed.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
Judy Martin
Public Relations
314-286-0105
Sign up for a free weekly e-mail on Medical Breakthroughs called
First to Know by clicking here.