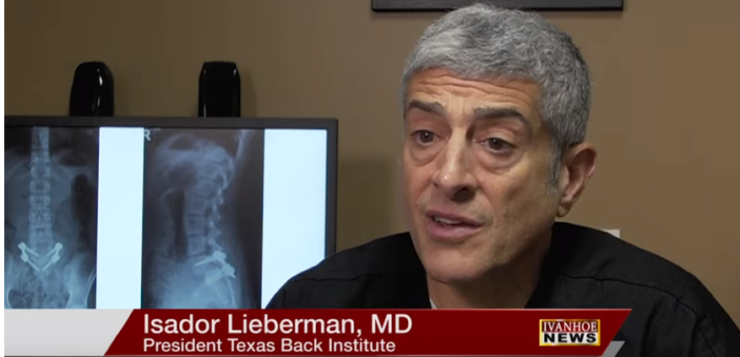
Isador Lieberman, MD, Orthopedic Surgeon at President Texas Back Institute talks about the BoneScapel and how it is improving spinal surgeries.
Interview conducted by Ivanhoe Broadcast News in May 2019.
We’re going to meet a young woman named Kaylee. Tell us what’s her problem and what did you need to do? I guess she’s a gymnast.
LIEBERMAN: Correct. So Kayleigh’s a young woman, teenager, who was very active with gym, with dance, who had what we call a isthmic spondylolisthesis That’s just a way of saying one bone has slipped forward on the other bone. And that was at the L5 S1 level where the bottom bone of the spine slid forward on top of the sacrum. When it does that, one, it hurts. It’s a mechanical pain. And two, the nerves get stretched and compressed so you get pain down the legs, weakness, numbness, tingling down the legs. And she had a very rapid progression which is the typical thing in teenagers. It starts off slow, but just like anything that’s going downhill as it goes, it goes faster and faster to the point where she was not able to participate in the activities that she loved doing.
Is it a type of scoliosis?
LIEBERMAN: It’s considered a spinal deformity. It’s not truly a scoliosis with a lateral bend, but it’s a forward translation of the two bones.
- So it’s slightly different, but it is a deformity of the spine.
LIEBERMAN: Yes.
Something that she was born with.
LIEBERMAN: Yeah. And there’s a lot of debate. And there’s obviously a genetic component to it. Yes, it’s something she was born with. But over time the developmental issues also lead to more problems. So the bone remodels and the sacrum becomes a downhill slope. So as L5 slides, it slides more over the top of it. So there’s nature and nurture involved in the progression of this issue.
Did her enthusiasm for gymnastics exercise and dance contribute to the problem?
LIEBERMAN: Again, very debatable. I feel, yeah. It probably did. The forces that she was putting on the bottom end of her spine, the vulnerable segment of spine, clearly weren’t able to accommodate to that. So I’m sure it did contribute to it. But if it didn’t happen last month, it would have probably happened a year or two years from now regardless with the way her spine was.
What would have been her prognosis without the advancements that you’ve been able to apply?
LIEBERMAN: She would have had to give up pretty much all her recreational and athletic endeavors. The spine would have not been stable enough to withstand the loads of pretty much most of her daily living activities. Sitting would have been difficult. Standing would have been difficult. Walking would be difficult. As it progresses and the nerves get more irritated, she would have neurological loss. She would start getting more weakness, numbness, tingling. And at some point that becomes irreversible. We don’t know when. We typically say somewhere around six months. If we see neurological signs, we want to get to it sooner rather than later because if we wait more than six months the nerves just can’t respond once you make more room for them. So she was looking at a very difficult life ahead of her with back pain and leg pain if this was left untreated.
And what did you decide that you wanted to do?
LIEBERMAN: On the basis of her current symptoms and on the basis of the rapid progression of the slip, I recommended that she consider an operation. Any time I make that recommendation, I weigh the risks versus the benefits. Spine surgery carries with it substantial risk. But in her case the benefits outweighed the risks. So I recommended to her and her parents – I said, this is not going to get better on its own. This is something that we have to rebuild for her.
With back surgery, sometimes it can save you and sometimes maybe it doesn’t. What’s your feeling about that overall?
LIEBERMAN: We do not want to do an operation unless we absolutely have to because of the risk profile of spinal surgery. What we do today is far better than what we were doing 15 years ago and 20 years ago. I also know what we’re going to be doing 15 years from now is going to make what we’re doing today look primitive. So we are getting better. The risk profile of spine surgery is decreasing, is diminishing, especially when we’re dealing with otherwise young, fit, healthy individuals. And we can intervene. We can act. We can address the issues earlier with less invasive methods so the recovery is better, the risk is less and the patients can return back to all the activities that they were doing beforehand with no restrictions.
So tell us about the procedure. There’s something new about this that makes it special, right?
LIEBERMAN: So what we need to do is to take the bones that have slipped forward, bring them back in line or lock them in place, and make more room for the nerves. So bringing back in line, that’s the realignment, the reduction of the deformity. Locking them in place – that’s the fusion. That’s like a broken arm that you put a cast on and the bone knits itself together to get solid again. That’s what we’re doing in the spine. We’re fusing that segment so it doesn’t continue to slip. And then we’ve got making more room for the nerves which is the decompression. So we get some decompression by realigning the spine but we get some decompression by removing some of the bone that was pushing on the nerves. The way we do it now we’re using a lot less invasive techniques so we can put the screws in to hold things in place, to facilitate that fusion. To lock it, there is an internal cast through what we call a percutaneous approach, meaning just with poke holes through the skin. And we use various robotic guidance technology to make sure we’re accurate in putting those in. We can do the fusion with multiple new biologics. We do use bone marrow and take the stem cells of that to generate the fusion itself. And in Caylee’s case we used her own bone that we cut and fashioned to fill in the gap where we rebuilt her spine. And we’ve got new tools now where I can be very precise with those bone cuts. And that’s the ultrasonic spine surgery that we’re now doing. So I can take a piece of bone that’s shaped kind of funny and I can carve it into a perfect block to fit exactly where I need it so the carpentry is precise to generate the fusion and to hold the alignment there. So we bring all of those things together and that’s what makes what we’re doing today better than when it was 15 years ago. But this is what we’re learning for the future. So I know I’m going to be able to do this even better 10 or 15 years from now for the next Kaylie that comes along.
The overall title of these types of stories, we call them medical breakthroughs. So if this is a medical breakthrough, tell me why.
LIEBERMAN: The breakthrough is with respect to the efficiency and accuracy of surgery. Traditionally, orthopedic surgeons would take an x ray and we’d say OK, we’ll cut bone here. We’ll put a screw here. We’ll do this this this and this. And we wouldn’t plan it. We’d get to the operating room and we just sort of try to get through it and then we look at the original X-ray, we’d look at our final X-ray and say it looks OK but it wasn’t exactly what we planned. It wasn’t done as efficiently as we could. I called those x rays trunk films because whenever I saw a picture like that I put it in the trunk of my car, and when I sold my car I wouldn’t empty the trunk because I didn’t want to see them again. But the medical breakthrough now is the ability to preoperatively plan and to use the tools to make you more efficient and more precise during surgery. So an operation like this that ten years ago would have taken me six to eight hours to do, I’m now doing an under three hours because we come to the operating room prepared and we have a suite of tools that facilitate the carpentry work that I need to do on the spine.
I like the way you equate it to carpentry or physical work. Heart doctors might be somewhere between an electrician and a plumber. So the analogy kind of works doesn’t it?
LIEBERMAN: It absolutely does work. And I look at myself as a little bit of an electrician and a lot of a carpenter. I am working on the spinal cord, the nerves, the nervous system. I’ve got to move all those wires all over the place safely, I’ve got to make sure we don’t damage any of them. So I have to know what the electrician has to know. The carpenter – he’s got to build it straight. He’s got to build it solid. There’s also a bit of engineering in there. I have to understand the biomechanics, just like a bridge builder has to understand the mechanics of building a bridge and where the supports are gonna be and the braces are going to be. I need to know that in the spine. So that all comes together in the work that we do in spinal surgery.
An old friend of mine had a saying that he liked to use – the carpenter’s adage – measure it twice, cut once. And that’s kind of what you’re talking about isn’t it?
LIEBERMAN: Yeah, absolutely. So I do spend a lot of time before surgery planning every surgery out. And then when I get to the operating room, before we start the case, the whole team, myself, my assistant, the scrub tech, the circuiting tech, the equipment tech – we look at the plan and we say this is what we’re going to do – a, b, c, d, e. And without elevating our stature beyond anything we deserve, when you see the team at work, it’s like an orchestra. Everybody knows their role. Everybody knows when to pipe in, when to pipe out, what to do at each point so it just becomes that much more efficient. So we’ve planned twice. We’ve measured twice. But we’re only doing the surgery once and spinal surgery is not like golf. You don’t get a mulligan with spinal surgery.
That’s good. So when did Kayleigh have the surgery. And how did it go? Was it within few months?
LIEBERMAN: I think she’s over a year now. We can find out. So she’s done real well. She came in very anxious, and her parents were very anxious, as any parents would be when their young child needs to have a spinal operation. But she had a good attitude about herself. She was, as you’ll see, very eloquent, very intelligent young woman, knew exactly what we were gonna do, understood what we were going to do, and was prepared for it and realized that she really did not have many other options for this. We got to the operating room and the surgery went really well for her. No complications. The next morning we had her up and moving. She said her legs felt better. Her back felt better. But the most important thing that she noticed was her posture. When the L5 bone slips forward on the sacrum the posture is to lean forward and really hyper arch your back. You can’t straighten up because if you try to straighten up you put more pressure on the nerves and the brain says we don’t want pressure on the nerves so it postures these young patients in this very awkward position. The next day when she stood up the parents looked at her, she looked at us, and said, “look at me I’m standing straight again”. And she just started dancing and doing everything from that day forward.
In terms of her activities, can she do anything that she couldn’t do before?
LIEBERMAN: My goal with surgery is to get my patients back to doing everything they need to do and want to do, of course, provided it’s legal. Now, in her case the dance and the gymnastics – she will be able to get back to doing all of that. Now she’s not going to be as flexible as she was before, but it’s going to be such a limited loss of flexibility that she’s not going to notice it. She’s not going to perceive that. Now, I do have to hold her back until the bone fuses. Things still have to heal and we still have to rehabilitate the muscles and get the muscle coordination there. But I expect she will be doing all that stuff without any restrictions for the rest of her life.
Elaborate a little bit on how you feel when you see this kind of result and how you see the development of your field and the future.
LIEBERMAN: Spine surgery is very, very unique in that when it doesn’t go well, it’s terrible. It really is bad. But when it does go well, it’s phenomenal. We don’t get the credit that we deserve as spine surgeons for a lot of the stuff that we do. And unfortunately that’s more related to the risk profile because we are working in a very high risk environment. We’re working with very delicate tissues and even the best of us run into issues. But the negative always gets amplified. The positive doesn’t. So for me, yeah. When I see her smile, when I see them doing things, and I’ve got a lot of young patients that are Olympic athletes, that have grown up to be firemen, policemen and executives and have achieved so much, it really is gratifying. And I consider them my children. It’s not much different. You just feel that inner pride that you are able to contribute and keep that individual’s life’s aspirations intact for them.
END OF INTERVIEW
This information is intended for additional research purposes only. It is not to be used as a prescription or advice from Ivanhoe Broadcast News, Inc. or any medical professional interviewed. Ivanhoe Broadcast News, Inc. assumes no responsibility for the depth or accuracy of physician statements. Procedures or medicines apply to different people and medical factors; always consult your physician on medical matters.
If you would like more information, please contact:
Audra Friis, PR
915-519-9577
audra@pascalecommunications.com
Sign up for a free weekly e-mail on Medical Breakthroughs called
First to Know by clicking here